Related Research Articles

Gastroenterology is the branch of medicine focused on the digestive system and its disorders. The digestive system consists of the gastrointestinal tract, sometimes referred to as the GI tract, which includes the esophagus, stomach, small intestine and large intestine as well as the accessory organs of digestion which include the pancreas, gallbladder, and liver.

Bile, or gall, is a yellow-green fluid produced by the liver of most vertebrates that aids the digestion of lipids in the small intestine. In humans, bile is primarily composed of water, produced continuously by the liver, and stored and concentrated in the gallbladder. After a human eats, this stored bile is discharged into the first section of the small intestine.

In vertebrates, the gallbladder, also known as the cholecyst, is a small hollow organ where bile is stored and concentrated before it is released into the small intestine. In humans, the pear-shaped gallbladder lies beneath the liver, although the structure and position of the gallbladder can vary significantly among animal species. It receives bile, produced by the liver, via the common hepatic duct, and stores it. The bile is then released via the common bile duct into the duodenum, where the bile helps in the digestion of fats.

Cholecystectomy is the surgical removal of the gallbladder. Cholecystectomy is a common treatment of symptomatic gallstones and other gallbladder conditions. In 2011, cholecystectomy was the eighth most common operating room procedure performed in hospitals in the United States. Cholecystectomy can be performed either laparoscopically, or via an open surgical technique.
A Klatskin tumor is a cholangiocarcinoma occurring at the confluence of the right and left hepatic bile ducts. The disease was named after Gerald Klatskin, who in 1965 described 15 cases and found some characteristics for this type of cholangiocarcinoma

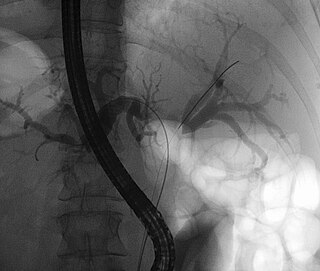
Endoscopic retrograde cholangiopancreatography (ERCP) is a technique that combines the use of endoscopy and fluoroscopy to diagnose and treat certain problems of the biliary or pancreatic ductal systems. It is primarily performed by highly skilled and specialty trained gastroenterologists. Through the endoscope, the physician can see the inside of the stomach and duodenum, and inject a contrast medium into the ducts in the biliary tree and pancreas so they can be seen on radiographs.

Cholangiocarcinoma, also known as bile duct cancer, is a type of cancer that forms in the bile ducts. Symptoms of cholangiocarcinoma may include abdominal pain, yellowish skin, weight loss, generalized itching, and fever. Light colored stool or dark urine may also occur. Other biliary tract cancers include gallbladder cancer and cancer of the ampulla of Vater.

Acute pancreatitis (AP) is a sudden inflammation of the pancreas. Causes, in order of frequency, include: a gallstone impacted in the common bile duct beyond the point where the pancreatic duct joins it; heavy alcohol use; systemic disease; trauma; and, in children, mumps. Acute pancreatitis may be a single event; it may be recurrent; or it may progress to chronic pancreatitis and/or pancreatic failure.

A pancreaticoduodenectomy, also known as a Whipple procedure, is a major surgical operation most often performed to remove cancerous tumours from the head of the pancreas. It is also used for the treatment of pancreatic or duodenal trauma, or chronic pancreatitis. Due to the shared blood supply of organs in the proximal gastrointestinal system, surgical removal of the head of the pancreas also necessitates removal of the duodenum, proximal jejunum, gallbladder, and, occasionally, part of the stomach.
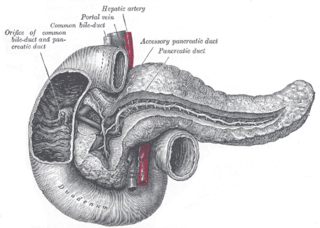
The pancreatic duct or duct of Wirsung is a duct joining the pancreas to the common bile duct. This supplies it with pancreatic juice from the exocrine pancreas, which aids in digestion.

A pancreatic pseudocyst is a circumscribed collection of fluid rich in pancreatic enzymes, blood, and non-necrotic tissue, typically located in the lesser sac of the abdomen. Pancreatic pseudocysts are usually complications of pancreatitis, although in children they frequently occur following abdominal trauma. Pancreatic pseudocysts account for approximately 75% of all pancreatic masses.

Magnetic resonance cholangiopancreatography (MRCP) is a medical imaging technique. It uses magnetic resonance imaging to visualize the biliary and pancreatic ducts non-invasively. This procedure can be used to determine whether gallstones are lodged in any of the ducts surrounding the gallbladder.

Ascending cholangitis, also known as acute cholangitis or simply cholangitis, is inflammation of the bile duct, usually caused by bacteria ascending from its junction with the duodenum. It tends to occur if the bile duct is already partially obstructed by gallstones.

Autoimmune Pancreatitis (AIP) is an increasingly recognized type of chronic pancreatitis that can be difficult to distinguish from pancreatic carcinoma but which responds to treatment with corticosteroids, particularly prednisone. Although autoimmune pancreatitis is quite rare, it constitutes an important clinical problem for both patients and their clinicians: the disease commonly presents itself as a tumorous mass which is diagnostically indistinguishable from pancreatic cancer, a disease that is much more common in addition to being very dangerous. Hence, some patients undergo pancreatic surgery, which is associated to substantial mortality and morbidity, out of the fear by patients and clinicians to undertreat a malignancy. However, surgery is not a good treatment for this condition as AIP responds well to immunosuppressive treatment. There are two categories of AIP: Type 1 and Type 2, each with distinct clinical profiles.

The major duodenal papilla is a rounded projection in the duodenum into which the common bile duct and pancreatic duct drain. The major duodenal papilla is, in most people, the primary mechanism for the secretion of bile and other enzymes that facilitate digestion.

Gallbladder diseases are diseases involving the gallbladder and is closely linked to biliary disease, with the most common cause being gallstones (cholelithiasis).

A persistent cloaca is a symptom of a complex anorectal congenital disorder, in which the rectum, vagina, and urinary tract meet and fuse, creating a cloaca, a single common channel.

Sphincter of Oddi dysfunction refers to a group of functional disorders leading to abdominal pain due to dysfunction of the Sphincter of Oddi: functional biliary sphincter of Oddi and functional pancreatic sphincter of Oddi disorder. The sphincter of Oddi is a sphincter muscle, a circular band of muscle at the bottom of the biliary tree which controls the flow of pancreatic juices and bile into the second part of the duodenum. The pathogenesis of this condition is recognized to encompass stenosis or dyskinesia of the sphincter of Oddi ; consequently the terms biliary dyskinesia, papillary stenosis, and postcholecystectomy syndrome have all been used to describe this condition. Both stenosis and dyskinesia can obstruct flow through the sphincter of Oddi and can therefore cause retention of bile in the biliary tree and pancreatic juice in the pancreatic duct.

The sphincter of Oddi, abbreviated as SO, is a muscular valve that in some animals, including humans, controls the flow of bile and pancreatic juice out of the gallbladder and pancreas respectively through the ampulla of Vater into the second part of the duodenum. It is named after Ruggero Oddi.

Biliary endoscopic sphincterotomy is a procedure where the sphincter of Oddi and the segment of the common bile duct where it enters the duodenum are cannulated and then cut with a sphincterotome, a device that includes a wire which cuts with an electric current (electrocautery).
References
- ↑ Kamisawa, Terumi; Honda, Goro (September 4, 2018). "Pancreaticobiliary Maljunction: Markedly High Risk for Biliary Cancer". Digestion. 99 (2). S. Karger AG: 123–125. doi: 10.1159/000490816 . ISSN 0012-2823. PMID 30179869.
- 1 2 Kamisawa, Terumi; Ando, Hisami; Hamada, Yoshinori; Fujii, Hideki; Koshinaga, Tsugumichi; Urushihara, Naoto; Itoi, Takao; Shimada, Hiroshi (December 5, 2013). "Diagnostic criteria for pancreaticobiliary maljunction 2013". Journal of Hepato-Biliary-Pancreatic Sciences. 21 (3). Wiley: 159–161. doi:10.1002/jhbp.57. ISSN 1868-6974. PMID 24307541.
- 1 2 Ono, Ayako; Arizono, Shigeki; Isoda, Hiroyoshi; Togashi, Kaori (2020). "Imaging of Pancreaticobiliary Maljunction". RadioGraphics. 40 (2): 378–392. doi:10.1148/rg.2020190108. ISSN 0271-5333. PMID 31951513.
- ↑ Csendes, A.; Kruse, A.; Funch-Jensen, P.; Øster, M.J.; Ørnsholt, J.; Amdrup, E. (1979). "Pressure measurements in the biliary and pancreatic duct systems in controls and in patients with gallstones, previous cholecystectomy, or common bile duct stones". Gastroenterology. 77 (6). Elsevier BV: 1203–1210. doi:10.1016/0016-5085(79)90158-6. ISSN 0016-5085. PMID 499707.
- ↑ Ando, Hisami; Ito, Takahiro; Nagaya, Masahiro; Watanabe, Yoshio; Seo, Takahiko; Kaneko, Kenitiro (1995). "Pancreaticobiliary maljunction without choledochal cysts in infants and children: Clinical features and surgical therapy". Journal of Pediatric Surgery. 30 (12). Elsevier BV: 1658–1662. doi:10.1016/0022-3468(95)90445-x. ISSN 0022-3468. PMID 8749917.
- ↑ Kanek, K; Ando, H; Ito, T; Watanabe, Y; Seo, T; Harada, T; Ito, F (June 1997). "Protein plugs cause symptoms in patients with choledochal cysts". The American Journal of Gastroenterology. 92 (6): 1018–1021. PMID 9177522.
- 1 2 Morine, Yuji; Shimada, Mitsuo; Takamatsu, Hideo; Araida, Tatsuo; Endo, Itaru; Kubota, Masayuki; Toki, Akira; Noda, Takuo; Matsumura, Toshinobu; Miyakawa, Shuichi; Ishibashi, Hiroki; Kamisawa, Terumi; Shimada, Hiroshi (2013). "Clinical features of pancreaticobiliary maljunction: update analysis of 2nd Japan-nationwide survey". Journal of Hepato-Biliary-Pancreatic Sciences. 20 (5): 472–480. doi:10.1007/s00534-013-0606-2. ISSN 1868-6974. PMID 23579999.
- ↑ Kamisawa, Terumi; Kaneko, Kenitiro; Itoi, Takao; Ando, Hisami (2017). "Pancreaticobiliary maljunction and congenital biliary dilatation". The Lancet Gastroenterology & Hepatology. 2 (8). Elsevier BV: 610–618. doi:10.1016/s2468-1253(17)30002-x. ISSN 2468-1253. PMID 28691687.
- ↑ Todani, Takuji; Urushihara, Naoto; Watanabe, Yasuhiro; Toki, Akira; Uemura, Sadashige; Sato, Yasuhisa; Morotomi, Yoshiki (1990). "Pseudopancreatitis in choledochal cyst in children: Intraoperative study of amylase levels in the serum". Journal of Pediatric Surgery. 25 (3). Elsevier BV: 303–306. doi:10.1016/0022-3468(90)90072-h. ISSN 0022-3468. PMID 1690281.
- 1 2 Matsumoto, Yoshiro; Fujii, Hideki; Itakura, Jun; Mogaki, Masatoshi; Matsuda, Masanori; Morozumi, Atsuro; Fujino, Masayuki A.; Suda, Koichi (2001). "Pancreaticobiliary maljunction: Etiologic concepts based on radiologic aspects". Gastrointestinal Endoscopy. 53 (6). Elsevier BV: 614–619. doi:10.1067/mge.2001.113920. ISSN 0016-5107. PMID 11323587.
- ↑ KAMISAWA, T; EGAWA, N; NAKAJIMA, H; TSURUTA, K; OKAMOTO, A; MATSUKAWA, M (2005). "Origin of the long common channel based on pancreatographic findings in pancreaticobiliary maljunction". Digestive and Liver Disease. 37 (5). Elsevier BV: 363–367. doi:10.1016/j.dld.2004.11.007. ISSN 1590-8658. PMID 15843087.
- ↑ Urushihara, Naoto; Hamada, Yoshinori; Kamisawa, Terumi; Fujii, Hideki; Koshinaga, Tsugumichi; Morotomi, Yoshiki; Saito, Takeshi; Itoi, Takao; Kaneko, Kenitiro; Fukuzawa, Hiroaki; Ando, Hisami (2017). "Classification of pancreaticobiliary maljunction and clinical features in children". Journal of Hepato-Biliary-Pancreatic Sciences. 24 (8): 449–455. doi: 10.1002/jhbp.485 . ISSN 1868-6974. PMID 28639336.
- ↑ Working Committee of Clinical Practice Guidelines for Pancreaticobiliary Maljunction; Kamisawa, Terumi; Ando, Hisami; Suyama, Masafumi; Shimada, Mitsuo; Morine, Yuji; Shimada, Hiroshi (2012). "Japanese clinical practice guidelines for pancreaticobiliary maljunction". Journal of Gastroenterology. 47 (7): 731–759. doi:10.1007/s00535-012-0611-2. ISSN 0944-1174. PMID 22722902.