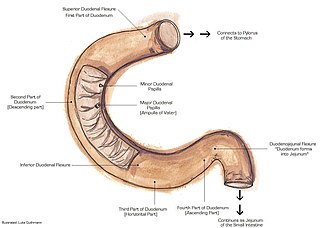
The duodenum is the first section of the small intestine in most higher vertebrates, including mammals, reptiles, and birds. In mammals, it may be the principal site for iron absorption. The duodenum precedes the jejunum and ileum and is the shortest part of the small intestine.

The small intestine or small bowel is an organ in the gastrointestinal tract where most of the absorption of nutrients from food takes place. It lies between the stomach and large intestine, and receives bile and pancreatic juice through the pancreatic duct to aid in digestion. The small intestine is about 5.5 metres long and folds many times to fit in the abdomen. Although it is longer than the large intestine, it is called the small intestine because it is narrower in diameter.

Cholecystectomy is the surgical removal of the gallbladder. Cholecystectomy is a common treatment of symptomatic gallstones and other gallbladder conditions. In 2011, cholecystectomy was the eighth most common operating room procedure performed in hospitals in the United States. Cholecystectomy can be performed either laparoscopically, or via an open surgical technique.

Acute pancreatitis (AP) is a sudden inflammation of the pancreas. Causes include a gallstone impacted in the common bile duct or the pancreatic duct, heavy alcohol use, systemic disease, trauma, elevated calcium levels, hypertriglyceridemia, certain medications, hereditary causes and, in children, mumps. Acute pancreatitis may be a single event, it may be recurrent, or it may progress to chronic pancreatitis and/or pancreatic failure.

A pancreaticoduodenectomy, also known as a Whipple procedure, is a major surgical operation most often performed to remove cancerous tumours from the head of the pancreas. It is also used for the treatment of pancreatic or duodenal trauma, or chronic pancreatitis. Due to the shared blood supply of organs in the proximal gastrointestinal system, surgical removal of the head of the pancreas also necessitates removal of the duodenum, proximal jejunum, gallbladder, and, occasionally, part of the stomach.
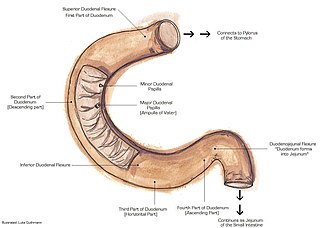
The suspensory muscle of duodenum is a thin muscle connecting the junction between the duodenum and jejunum, as well as the duodenojejunal flexure to connective tissue surrounding the superior mesenteric and coeliac arteries. The suspensory muscle most often connects to both the third and fourth parts of the duodenum, as well as the duodenojejunal flexure, although the attachment is quite variable.
Intestinal malrotation is a congenital anomaly of rotation of the midgut. It occurs during the first trimester as the fetal gut undergoes a complex series of growth and development. Malrotation can lead to a dangerous complication called volvulus, in which cases emergency surgery is indicated. Malrotation can refer to a spectrum of abnormal intestinal positioning, often including:
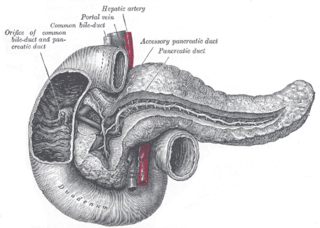
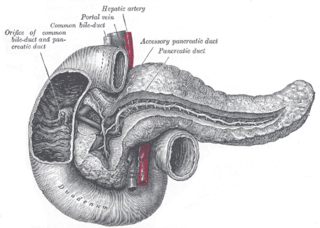
The pancreatic duct or duct of Wirsung is a duct joining the pancreas to the common bile duct. This supplies it with pancreatic juice from the exocrine pancreas, which aids in digestion.

A pancreatic pseudocyst is a circumscribed collection of fluid rich in pancreatic enzymes, blood, and non-necrotic tissue, typically located in the lesser sac of the abdomen. Pancreatic pseudocysts are usually complications of pancreatitis, although in children they frequently occur following abdominal trauma. Pancreatic pseudocysts account for approximately 75% of all pancreatic masses.

Pancreas divisum is a congenital anomaly in the anatomy of the ducts of the pancreas in which a single pancreatic duct is not formed, but rather remains as two distinct dorsal and ventral ducts. Most individuals with pancreas divisum remain without symptoms or complications. A minority of people with pancreatic divisum may develop episodes of abdominal pain, nausea or vomiting due to acute or chronic pancreatitis. The presence of pancreas divisum is usually identified with cross sectional diagnostic imaging, such as endoscopic retrograde cholangiopancreatography (ERCP) or magnetic resonance cholangiopancreatography (MRCP). In some cases, it may be detected intraoperatively. If no symptoms or complications are present, then treatment is not necessary. However, if there is recurrent pancreatitis, then a sphincterotomy of the minor papilla may be indicated.

Ascending cholangitis, also known as acute cholangitis or simply cholangitis, is inflammation of the bile duct, usually caused by bacteria ascending from its junction with the duodenum. It tends to occur if the bile duct is already partially obstructed by gallstones.

Hemosuccus pancreaticus is a rare cause of hemorrhage in the gastrointestinal tract. It is caused by a bleeding source in the pancreas, pancreatic duct, or structures adjacent to the pancreas, such as the splenic artery, that bleed into the pancreatic duct, which is connected with the bowel at the duodenum, the first part of the small intestine. Patients with hemosuccus may develop symptoms of gastrointestinal hemorrhage, such as blood in the stools, maroon stools, or melena, which is a dark, tarry stool caused by digestion of red blood cells. They may also develop abdominal pain. It is associated with pancreatitis, pancreatic cancer and aneurysms of the splenic artery. Hemosuccus may be identified with endoscopy (esophagogastroduodenoscopy), where fresh blood may be seen from the pancreatic duct. Alternatively, angiography may be used to inject the celiac axis to determine the blood vessel that is bleeding. This may also be used to treat hemosuccus, as embolization of the end vessel may terminate the hemorrhage. However, a distal pancreatectomy—surgery to remove of the tail of the pancreas—may be required to stop the hemorrhage.

An accessory spleen is a small nodule of splenic tissue found apart from the main body of the spleen. Accessory spleens are found in approximately 10 percent of the population and are typically around 1 centimetre in diameter. They may resemble a lymph node or a small spleen. They form either by the result of developmental anomalies or trauma. They are medically significant in that they may result in interpretation errors in diagnostic imaging or continued symptoms after therapeutic splenectomy. Polysplenia is the presence of multiple accessory spleens rather than one normal spleen.

Duodenal atresia is the congenital absence or complete closure of a portion of the lumen of the duodenum. It causes increased levels of amniotic fluid during pregnancy (polyhydramnios) and intestinal obstruction in newborn babies. Newborns present with bilious or non-bilous vomiting within the first 24 to 48 hours after birth, typically after their first oral feeding. Radiography shows a distended stomach and distended duodenum, which are separated by the pyloric valve, a finding described as the double-bubble sign.
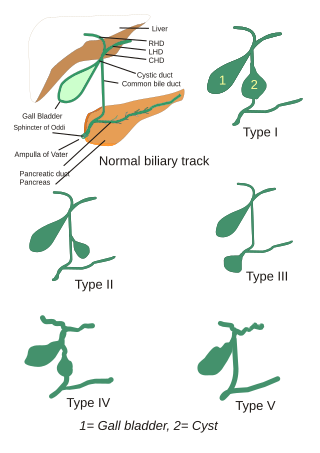
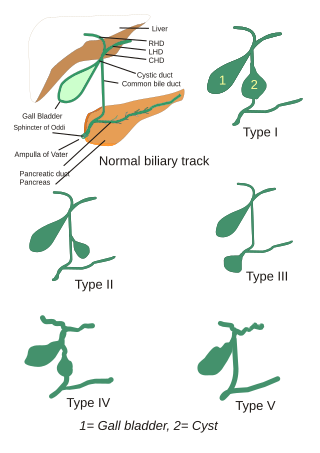
Choledochal cysts are congenital conditions involving cystic dilatation of bile ducts. They are uncommon in western countries but not as rare in East Asian nations like Japan and China.
Biliary dyskinesia is a disorder of some component of biliary part of the digestive system in which bile cannot physically move in the proper direction through the tubular biliary tract. It most commonly involves abnormal biliary tract peristalsis muscular coordination within the gallbladder in response to dietary stimulation of that organ to squirt the liquid bile through the common bile duct into the duodenum. Ineffective peristaltic contraction of that structure produces postprandial right upper abdominal pain (cholecystodynia) and almost no other problem. When the dyskinesia is localized at the biliary outlet into the duodenum just as increased tonus of that outlet sphincter of Oddi, the backed-up bile can cause pancreatic injury with abdominal pain more toward the upper left side. In general, biliary dyskinesia is the disturbance in the coordination of peristaltic contraction of the biliary ducts, and/or reduction in the speed of emptying of the biliary tree into the duodenum.
Megaduodenum is a congenital or acquired dilation and elongation of the duodenum with hypertrophy of all layers that presents as a feeling of gastric fullness, abdominal pain, belching, heartburn, and nausea with vomiting sometimes of food eaten 24 hours prior.
Neonatal bowel obstruction (NBO) or neonatal intestinal obstruction is the most common surgical emergency in the neonatal period. It may occur due to a variety of conditions and has an excellent outcome based on timely diagnosis and appropriate intervention.

In radiology, the double bubble sign is a feature of pediatric imaging seen on radiographs or prenatal ultrasound in which two air filled bubbles are seen in the abdomen, representing two discontiguous loops of bowel in a proximal, or 'high,' small bowel obstruction. The finding is typically pathologic, and implies either duodenal atresia, duodenal web, annular pancreas, or on occasion midgut volvulus, a distinction that requires close clinical correlation and, in most cases, surgical intervention.
Afferent loop syndrome is an uncommon side effect of gastric surgery. The afferent loop is made up of a segment of duodenum and/or proximal jejunum located upstream of a double-barrel gastrojejunostomy anastomosis. Abdominal pain and distension are signs of increased intraluminal pressure resulting from the accumulation of enteric secretions in the obstructed afferent loop.