Related Research Articles

Acetylcholine (ACh) is an organic compound that functions in the brain and body of many types of animals as a neurotransmitter. Its name is derived from its chemical structure: it is an ester of acetic acid and choline. Parts in the body that use or are affected by acetylcholine are referred to as cholinergic. Substances that increase or decrease the overall activity of the cholinergic system are called cholinergics and anticholinergics, respectively.
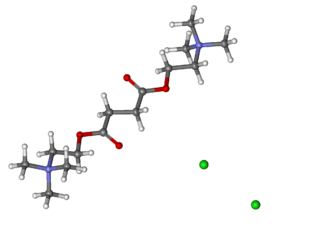
Suxamethonium chloride, also known as suxamethonium or succinylcholine, or simply sux by medical abbreviation, is a medication used to cause short-term paralysis as part of general anesthesia. This is done to help with tracheal intubation or electroconvulsive therapy. It is administered by injection, either into a vein or into a muscle. When used in a vein, onset of action is generally within one minute and effects last for up to 10 minutes.

Procaine is a local anesthetic drug of the amino ester group. It is most commonly used in dental procedures to numb the area around a tooth and is also used to reduce the pain of intramuscular injection of penicillin. Owing to the ubiquity of the trade name Novocain or Novocaine, in some regions, procaine is referred to generically as novocaine. It acts mainly as a sodium channel blocker. Today, it is used therapeutically in some countries due to its sympatholytic, anti-inflammatory, perfusion-enhancing, and mood-enhancing effects.

The enzyme cholinesterase (EC 3.1.1.8, choline esterase; systematic name acylcholine acylhydrolase) catalyses the hydrolysis of choline-based esters:

An anesthetic or anaesthetic is a drug used to induce anesthesia — in other words, to result in a temporary loss of sensation or awareness. They may be divided into two broad classes: general anesthetics, which result in a reversible loss of consciousness, and local anesthetics, which cause a reversible loss of sensation for a limited region of the body without necessarily affecting consciousness.

Chlorfenvinphos is the common name of an organophosphorus compound that was widely used as an insecticide and an acaricide. The molecule itself can be described as an enol ester derived from dichloroacetophenone and diethylphosphonic acid. Chlorfenvinphos has been included in many products since its first use in 1963. However, because of its toxic effect as a cholinesterase inhibitor it has been banned in several countries, including the United States and the European Union. Its use in the United States was cancelled in 1991.
In advanced airway management, rapid sequence induction (RSI) – also referred to as rapid sequence intubation or as rapid sequence induction and intubation (RSII) or as crash induction – is a special process for endotracheal intubation that is used where the patient is at a high risk of pulmonary aspiration. It differs from other techniques for inducing general anesthesia in that several extra precautions are taken to minimize the time between giving the induction drugs and securing the tube, during which period the patient's airway is essentially unprotected.
Benzonatate, sold under the brand name Tessalon among others, is a medication that is used for the symptomatic relief of cough. It is taken by mouth. Use is not recommended in those under the age of ten. Effects generally begin within 20 minutes and last up to eight hours.

Curare is a common name for various alkaloid arrow poisons originating from plant extracts. Used as a paralyzing agent by indigenous peoples in Central and South America for hunting and for therapeutic purposes, curare only becomes active when it contaminates a wound. These poisons cause weakness of the skeletal muscles and, when administered in a sufficient dose, eventual death by asphyxiation due to paralysis of the diaphragm. Curare is prepared by boiling the bark of one of the dozens of plant sources, leaving a dark, heavy paste that can be applied to arrow or dart heads. In medicine, curare has been used as a treatment for tetanus and strychnine poisoning and as a paralyzing agent for surgical procedures.

Neuromuscular-blocking drugs block neuromuscular transmission at the neuromuscular junction, causing paralysis of the affected skeletal muscles. This is accomplished via their action on the post-synaptic acetylcholine (Nm) receptors.
A cholinergic crisis is an over-stimulation at a neuromuscular junction due to an excess of acetylcholine (ACh), as a result of the inactivity of the AChE enzyme, which normally breaks down acetylcholine.

Mivacurium chloride is a short-duration non-depolarizing neuromuscular-blocking drug or skeletal muscle relaxant in the category of non-depolarizing neuromuscular-blocking drugs, used adjunctively in anesthesia to facilitate endotracheal intubation and to provide skeletal muscle relaxation during surgery or mechanical ventilation.

Doxacurium chloride is a neuromuscular-blocking drug or skeletal muscle relaxant in the category of non-depolarizing neuromuscular-blocking drugs, used adjunctively in anesthesia to provide skeletal muscle relaxation during surgery or mechanical ventilation. Unlike a number of other related skeletal muscle relaxants, it is rarely used adjunctively to facilitate endotracheal intubation.

Butyrylcholinesterase, also known as BChE, BuChE, BuChase, pseudocholinesterase, or plasma (cholin)esterase, is a nonspecific cholinesterase enzyme that hydrolyses many different choline-based esters. In humans, it is made in the liver, found mainly in blood plasma, and encoded by the BCHE gene.

Acetylcholinesterase (HGNC symbol ACHE; EC 3.1.1.7; systematic name acetylcholine acetylhydrolase), also known as AChE, AChase or acetylhydrolase, is the primary cholinesterase in the body. It is an enzyme that catalyzes the breakdown of acetylcholine and some other choline esters that function as neurotransmitters:
Neuromuscular junction disease is a medical condition where the normal conduction through the neuromuscular junction fails to function correctly.

Acetylcholinesterase inhibitors (AChEIs) also often called cholinesterase inhibitors, inhibit the enzyme acetylcholinesterase from breaking down the neurotransmitter acetylcholine into choline and acetate, thereby increasing both the level and duration of action of acetylcholine in the central nervous system, autonomic ganglia and neuromuscular junctions, which are rich in acetylcholine receptors. Acetylcholinesterase inhibitors are one of two types of cholinesterase inhibitors; the other being butyryl-cholinesterase inhibitors. Acetylcholinesterase is the primary member of the cholinesterase enzyme family.
Dibucaine, also known as cinchocaine, is an amino amide local anesthetic. When administered to humans intravenously, it is capable of inhibiting the plasma cholinesterase (butyrylcholinesterase) enzyme. The dibucaine number is used to differentiate individuals who have substitution mutations of the enzyme's gene, resulting in decreased enzyme function.

Postoperative residual curarization (PORC) or residual neuromuscular blockade (RNMB) is a residual paresis after emergence from general anesthesia that may occur with the use of neuromuscular-blocking drugs. Today residual neuromuscular blockade is defined as a train of four ratio of less than 0.9 when measuring the response to ulnar nerve stimulation at the adductor pollicis muscle using mechanomyography or electromyography. A meta-analysis reported that the incidence of residual neuromuscular paralysis was 41% in patients receiving intermediate neuromuscular blocking agents during anaesthesia. It is possible that > 100,000 patients annually in the USA alone, are at risk of adverse events associated with undetected residual neuromuscular blockade. Neuromuscular function monitoring and the use of the appropriate dosage of sugammadex to reverse blockade produced by rocuronium can reduce the incidence of postoperative residual curarization. In this study, with usual care group receiving reversal with neostigmine resulted in a residual blockade rate of 43%.
Neuromuscular blocking agents, or in abbreviation, NMBAs, are chemical agents that paralyse skeletal muscles by blocking the movement of neurotransmitter at the neuromuscular junction. They are often used during general anesthesia to optimize intubating and surgical conditions, specifically to facilitate endotracheal intubation. This class of medications helps to reduce patient movement, breathing, or ventilator dyssynchrony and allows lower insufflation pressures during laparoscopy including the generation of nerve impulses. It has several indications for use in the intense care unit. It can help reduce hoarseness in voice as well as injury to the vocal cord during intubation. In addition, it plays an important role in facilitating mechanical ventilation in patients with poor lung function. In the following section, neuromuscular blocking agent's history, usages, mechanisms, side effects, interactions and pharmacology will further be elaborated and discussed.
References
- ↑ Maiorana, A; Roach Jr, RB (2003). "Heterozygous pseudocholinesterase deficiency: A case report and review of the literature". Journal of Oral and Maxillofacial Surgery. 61 (7): 845–7. doi:10.1016/S0278-2391(03)00163-0. PMID 12856264.
- ↑ Alexander, Daniel R. (2002). Pseudocholinesterase deficiency. Retrieved Mar. 13, 2007.
- ↑ title= Ottawa Anaesthesia Primer |chapter=Neuromuscular blocking agents |year=2012 |pages=150
- 1 2 title=Syndromes: Rapid Recognition and Perioperative Implications | Cholineseterase deficiency
- 1 2 3 4 5 6 Li, B.; Duysen, E. G.; Carlson, M.; Lockridge, O. (2007). "The Butyrylcholinesterase Knockout Mouse as a Model for Human Butyrylcholinesterase Deficiency". Journal of Pharmacology and Experimental Therapeutics. 324 (3): 1146–54. doi:10.1124/jpet.107.133330. PMID 18056867. S2CID 12430774.
- ↑ Daniel R Alexander. (2006). "Pseudocholinesterase Deficiency". eMedicine Retrieved June 16, 2008
- ↑ "Cholinesterase Test". Lab Tests Online. Retrieved 21 July 2014.
- ↑ Manoharan, I; Wieseler, S; Layer, PG; Lockridge, O; Boopathy, R (2006). "Naturally occurring mutation Leu307Pro of human butyrylcholinesterase in the Vysya community of India". Pharmacogenetics and Genomics. 16 (7): 461–8. doi:10.1097/01.fpc.0000197464.37211.77. PMID 16788378. S2CID 21915244.
- ↑ Cedars-Sinai Medical Genetics Institute. (2009). "Genetic Screening in the Persian Jewish Community". Retrieved July 20, 2011.