| Schober's test | |
|---|---|
| Purpose | ability to flex lower back |

Schober's test is a physical examination used in family medicine, physical medicine and rehabilitation, rheumatology to measure the ability of a patient to flex the lower back.
| Schober's test | |
|---|---|
| Purpose | ability to flex lower back |

Schober's test is a physical examination used in family medicine, physical medicine and rehabilitation, rheumatology to measure the ability of a patient to flex the lower back.
While the patient is in a standing position the examiner makes a mark approximately at the level of L5 (fifth lumbar vertebra). Two points are marked: 5 cm below and 10 cm above this point (for a total of 15 cm distance). Then the patient is asked to touch his/her toes while keeping the knees straight. If the distance of the two points do not increase by at least 5 cm (with the total distance greater than 20 cm), then this is a sign of restriction in the lumbar flexion. [1] This can be useful in examining a patient suspected of ankylosing spondylitis.
The test was first described in 1937 by Dr Paul Schober (March 11, 1865 - August 22, 1943), a German physician. [2] [3]

Lumbar puncture (LP), also known as a spinal tap, is a medical procedure in which a needle is inserted into the spinal canal, most commonly to collect cerebrospinal fluid (CSF) for diagnostic testing. The main reason for a lumbar puncture is to help diagnose diseases of the central nervous system, including the brain and spine. Examples of these conditions include meningitis and subarachnoid hemorrhage. It may also be used therapeutically in some conditions. Increased intracranial pressure is a contraindication, due to risk of brain matter being compressed and pushed toward the spine. Sometimes, lumbar puncture cannot be performed safely. It is regarded as a safe procedure, but post-dural-puncture headache is a common side effect if a small atraumatic needle is not used.

The Lachman test is a clinical test used to diagnose injury of the anterior cruciate ligament (ACL). It is recognized as reliable, sensitive, and usually superior to the anterior drawer test.
Spondylosis is the degeneration of the vertebral column from any cause. In the more narrow sense it refers to spinal osteoarthritis, the age-related degeneration of the spinal column, which is the most common cause of spondylosis. The degenerative process in osteoarthritis chiefly affects the vertebral bodies, the neural foramina and the facet joints. If severe, it may cause pressure on the spinal cord or nerve roots with subsequent sensory or motor disturbances, such as pain, paresthesia, imbalance, and muscle weakness in the limbs.

Spondylolisthesis is the displacement of one spinal vertebra compared to another. While some medical dictionaries define spondylolisthesis specifically as the forward or anterior displacement of a vertebra over the vertebra inferior to it, it is often defined in medical textbooks as displacement in any direction. Spondylolisthesis is graded based upon the degree of slippage of one vertebral body relative to the subsequent adjacent vertebral body. Spondylolisthesis is classified as one of the six major etiologies: degenerative, traumatic, dysplastic, isthmic, pathologic, or post-surgical. Spondylolisthesis most commonly occurs in the lumbar spine, primarily at the L5-S1 level, with the L5 vertebral body anteriorly translating over the S1 vertebral body.

A nerve conduction study (NCS) is a medical diagnostic test commonly used to evaluate the function, especially the ability of electrical conduction, of the motor and sensory nerves of the human body. These tests may be performed by medical specialists such as clinical neurophysiologists, physical therapists, physiatrists, and neurologists who subspecialize in electrodiagnostic medicine. In the United States, neurologists and physiatrists receive training in electrodiagnostic medicine as part of residency training and in some cases acquire additional expertise during a fellowship in clinical neurophysiology, electrodiagnostic medicine, or neuromuscular medicine. Outside the US, clinical neurophysiologists learn needle EMG and NCS testing.
Gaenslen's test, also known as Gaenslen's maneuver, is a medical test used to detect musculoskeletal abnormalities and primary-chronic inflammation of the lumbar vertebrae and sacroiliac joint. This test is often used to test for spondyloarthritis, sciatica, or other forms of rheumatism, and is often performed during checkup visits in patients who have been diagnosed with one of the former disorders. It is named after Frederick Julius Gaenslen, the orthopedic surgeon who invented the test. This test is often performed alongside Patrick's test and Yeoman's test.

Spondylolysis is a defect or stress fracture in the pars interarticularis of the vertebral arch. The vast majority of cases occur in the lower lumbar vertebrae (L5), but spondylolysis may also occur in the cervical vertebrae.
The knee examination, in medicine and physiotherapy, is performed as part of a physical examination, or when a patient presents with knee pain or a history that suggests a pathology of the knee joint.
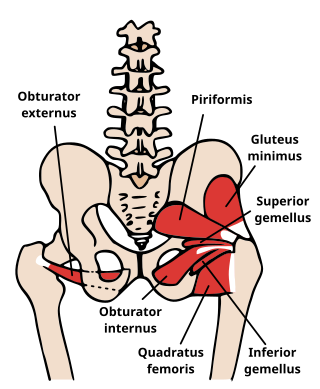
The obturator sign, also called Cope's obturator test, is an indicator of irritation to the obturator internus muscle.
In medicine, physiotherapy, chiropractic, and osteopathy the hip examination, or hip exam, is undertaken when a patient has a complaint of hip pain and/or signs and/or symptoms suggestive of hip joint pathology. It is a physical examination maneuver.

A spinal disc herniation is an injury to the intervertebral disc between two spinal vertebrae, usually caused by excessive strain or trauma to the spine. It may result in back pain, pain or sensation in different parts of the body, and physical disability. The most conclusive diagnostic tool for disc herniation is MRI, and treatment may range from painkillers to surgery. Protection from disc herniation is best provided by core strength and an awareness of body mechanics including good posture.
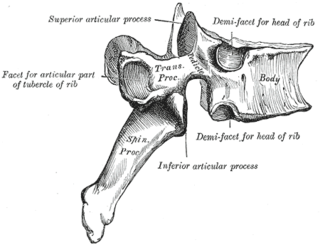
The facet joints are a set of synovial, plane joints between the articular processes of two adjacent vertebrae. There are two facet joints in each spinal motion segment and each facet joint is innervated by the recurrent meningeal nerves.

Radiculopathy, also commonly referred to as pinched nerve, refers to a set of conditions in which one or more nerves are affected and do not work properly. Radiculopathy can result in pain, weakness, altered sensation (paresthesia) or difficulty controlling specific muscles. Pinched nerves arise when surrounding bone or tissue, such as cartilage, muscles or tendons, put pressure on the nerve and disrupt its function.

The straight leg raise is a test that can be performed during a physical examination, with the leg being lifted actively by the patient or passively by the clinician. If the straight leg raise is done actively by the patient it is a test of functional leg strength, particularly the rectus femoris element of the quadriceps. If carried out passively, it is used to determine whether a patient with low back pain has an underlying nerve root sensitivity, often located at L5. The rest of this article relates to the passive version of the test.
Neurogenic claudication (NC), also known as pseudoclaudication, is the most common symptom of lumbar spinal stenosis (LSS) and describes intermittent leg pain from impingement of the nerves emanating from the spinal cord. Neurogenic means that the problem originates within the nervous system. Claudication, from the Latin word for to limp, refers to painful cramping or weakness in the legs. NC should therefore be distinguished from vascular claudication, which stems from a circulatory problem rather than a neural one.
A GALS screen is an examination used by doctors and other healthcare professionals to detect locomotor abnormalities and functional disability relating to gait, arms, legs and the spine.

The Thomas test is a physical examination test, named after the Welsh orthopaedic surgeon, Hugh Owen Thomas (1834–1891), to rule out hip flexion contracture and psoas syndrome.
Ober's test is used in physical examination to identify tightness of the iliotibial band . During the test, the patient lies on his/her side with the unaffected leg on the bottom with their shoulder and pelvis in line. The lower hip and knee can be in a flexed position to take out any lordosis of the lumbar spine.

The term sacroiliac joint dysfunction refers to abnormal motion in the sacroiliac joint, either too much motion or too little motion, that causes pain in this region.
Williams flexion exercises (WFE) – also called Williams lumbar flexion exercises – are a set of related physical exercises intended to enhance lumbar flexion, avoid lumbar extension, and strengthen the abdominal and gluteal musculature in an effort to manage low back pain non-surgically. The system was first devised in 1937 by Dallas orthopedic surgeon Dr. Paul C. Williams.