Inclusion body myositis (IBM) is the most common inflammatory muscle disease in older adults. The disease is characterized by slowly progressive weakness and wasting of both proximal muscles and distal muscles, most apparent in the finger flexors and knee extensors. IBM is often confused with an entirely different class of diseases, called hereditary inclusion body myopathies (hIBM). The "M" in hIBM is an abbreviation for "myopathy" while the "M" in IBM is for "myositis". In IBM, two processes appear to occur in the muscles in parallel, one autoimmune and the other degenerative. Inflammation is evident from the invasion of muscle fibers by immune cells. Degeneration is characterized by the appearance of holes, deposits of abnormal proteins, and filamentous inclusions in the muscle fibers. sIBM is a rare disease, with a prevalence ranging from 1 to 71 individuals per million.

Myasthenia gravis (MG) is a long-term neuromuscular junction disease that leads to varying degrees of skeletal muscle weakness. The most commonly affected muscles are those of the eyes, face, and swallowing. It can result in double vision, drooping eyelids, and difficulties in talking and walking. Onset can be sudden. Those affected often have a large thymus or develop a thymoma.

Myalgia or muscle pain is a painful sensation evolving from muscle tissue. It is a symptom of many diseases. The most common cause of acute myalgia is the overuse of a muscle or group of muscles; another likely cause is viral infection, especially when there has been no injury.

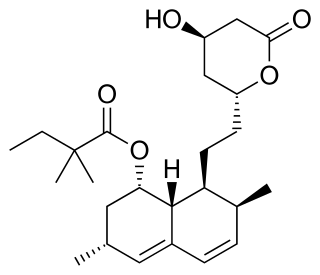
Statins are a class of medications that lower cholesterol. They are prescribed typically to people who are at high risk of cardiovascular disease.
A cramp is a sudden, involuntary, painful skeletal muscle contraction or overshortening associated with electrical activity; while generally temporary and non-damaging, they can cause significant pain and a paralysis-like immobility of the affected muscle. A cramp usually goes away on its own over a period of several seconds or (sometimes) minutes. Cramps are common and tend to occur at rest, usually at night. They are also often associated with pregnancy, physical exercise or overexertion, and age ; in such cases, cramps are called idiopathic, because there is no underlying pathology. In addition to those benign conditions cramps are also associated with many pathological conditions.

Atorvastatin is a statin medication used to prevent cardiovascular disease in those at high risk and to treat abnormal lipid levels. For the prevention of cardiovascular disease, statins are a first-line treatment. It is taken by mouth.
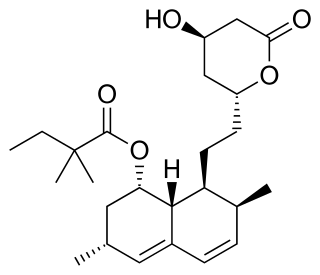
Simvastatin, sold under the brand name Zocor among others, is a statin, a type of lipid-lowering medication. It is used along with exercise, diet, and weight loss to decrease elevated lipid levels. It is also used to decrease the risk of heart problems in those at high risk. It is taken by mouth.

Cerivastatin is a synthetic member of the class of statins used to lower cholesterol and prevent cardiovascular disease. It was marketed by the pharmaceutical company Bayer A.G. in the late 1990s, competing with Pfizer's highly successful atorvastatin (Lipitor). Cerivastatin was voluntarily withdrawn from the market worldwide in 2001, due to reports of fatal rhabdomyolysis.

HMG-CoA reductase is the rate-controlling enzyme of the mevalonate pathway, the metabolic pathway that produces cholesterol and other isoprenoids. HMGCR catalyzes the conversion of HMG-CoA to mevalonic acid, a necessary step in the biosynthesis of cholesterol. Normally in mammalian cells this enzyme is competitively suppressed so that its effect is controlled. This enzyme is the target of the widely available cholesterol-lowering drugs known collectively as the statins, which help treat dyslipidemia.

Dermatomyositis (DM) is a long-term inflammatory disorder which affects the skin and the muscles. Its symptoms are generally a skin rash and worsening muscle weakness over time. These may occur suddenly or develop over months. Other symptoms may include weight loss, fever, lung inflammation, or light sensitivity. Complications may include calcium deposits in muscles or skin.
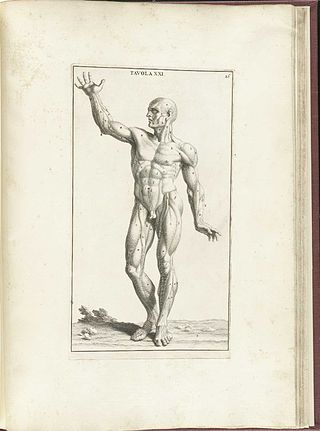
In medicine, myopathy is a disease of the muscle in which the muscle fibers do not function properly. Myopathy means muscle disease. This meaning implies that the primary defect is within the muscle, as opposed to the nerves or elsewhere.

Polymyositis (PM) is a type of chronic inflammation of the muscles related to dermatomyositis and inclusion body myositis. Its name is derived from poly- 'many' myos- 'muscle' and -itis 'inflammation'. The inflammation of polymyositis is mainly found in the endomysial layer of skeletal muscle, whereas dermatomyositis is characterized primarily by inflammation of the perimysial layer of skeletal muscles.
Microscopic polyangiitis is an autoimmune disease characterized by a systemic, pauci-immune, necrotizing, small-vessel vasculitis without clinical or pathological evidence of granulomatous inflammation.

Myositis is a rarely-encountered medical condition characterized by inflammation affecting the muscles. The manifestations of this condition may include skin issues, muscle weakness, and the potential involvement of other organs. Additionally, systemic symptoms like weight loss, fatigue, and low-grade fever can manifest in individuals with myositis.
Mixed connective tissue disease (MCTD) is a systemic autoimmune disease that shares characteristics with at least two other systemic autoimmune diseases, including systemic sclerosis (Ssc), systemic lupus erythematosus (SLE), polymyositis/dermatomyositis (PM/DM), and rheumatoid arthritis. The idea behind the "mixed" disease is that this specific autoantibody is also present in other autoimmune diseases such as systemic lupus erythematosus, polymyositis, scleroderma, etc. MCTD was characterized as an individual disease in 1972 by Sharp et al., and the term was introduced by Leroy in 1980.

Drug-induced lupus erythematosus is an autoimmune disorder caused by chronic use of certain drugs. These drugs cause an autoimmune response producing symptoms similar to those of systemic lupus erythematosus (SLE). There are 38 known medications to cause DIL but there are three that report the highest number of cases: hydralazine, procainamide, and quinidine. While the criteria for diagnosing DIL has not been thoroughly established, symptoms of DIL typically present as muscle pain and joint pain. Generally, the symptoms recede after discontinuing use of the drugs.
Scleromyositis, is an autoimmune disease. People with scleromyositis have symptoms of both systemic scleroderma and either polymyositis or dermatomyositis, and is therefore considered an overlap syndrome. Although it is a rare disease, it is one of the more common overlap syndromes seen in scleroderma patients, together with MCTD and Antisynthetase syndrome. Autoantibodies often found in these patients are the anti-PM/Scl (anti-exosome) antibodies.

Inflammatory myopathy, also known as idiopathic inflammatory myopathy (IIM), is disease featuring muscle weakness, inflammation of muscles (myositis), and in some types, muscle pain (myalgia). The cause of much inflammatory myopathy is unknown (idiopathic), and such cases are classified according to their symptoms and signs, electromyography, MRI, and laboratory findings. It can also be associated with underlying cancer. The main classes of idiopathic inflammatory myopathy are polymyositis (PM), dermatomyositis (DM), inclusion-body myositis (IBM), immune-mediated necrotising myopathy (IMNM), and focal autoimmune myositis.
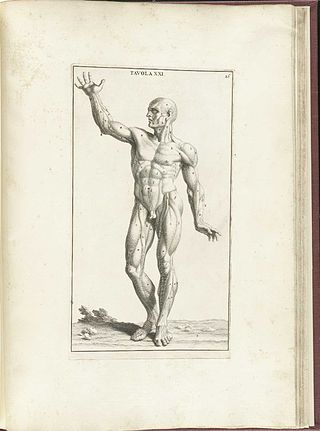
Acquired non-inflammatory myopathy (ANIM) is a neuromuscular disorder primarily affecting skeletal muscle, most commonly in the limbs of humans, resulting in a weakness or dysfunction in the muscle. A myopathy refers to a problem or abnormality with the myofibrils, which compose muscle tissue. In general, non-inflammatory myopathies are a grouping of muscular diseases not induced by an autoimmune-mediated inflammatory pathway. These muscular diseases usually arise from a pathology within the muscle tissue itself rather than the nerves innervating that tissue. ANIM has a wide spectrum of causes which include drugs and toxins, nutritional imbalances, acquired metabolic dysfunctions such as an acquired defect in protein structure, and infections.

Antisynthetase syndrome (ASS) is a multisystematic autoimmune disease associated with inflammatory myositis, interstitial lung disease, and antibodies directed against various synthetases of aminoacyl-transfer RNA. Other common symptoms include mechanic's hands, Raynaud's phenomenon, arthritis, and fever.