Anosmia, also known as smell blindness, is the loss of the ability to detect one or more smells. Anosmia may be temporary or permanent. It differs from hyposmia, which is a decreased sensitivity to some or all smells.

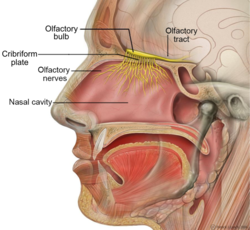
The olfactory nerve, also known as the first cranial nerve, cranial nerve I, or simply CN I, is a cranial nerve that contains sensory nerve fibers relating to the sense of smell.

The olfactory bulb is a neural structure of the vertebrate forebrain involved in olfaction, the sense of smell. It sends olfactory information to be further processed in the amygdala, the orbitofrontal cortex (OFC) and the hippocampus where it plays a role in emotion, memory and learning. The bulb is divided into two distinct structures: the main olfactory bulb and the accessory olfactory bulb. The main olfactory bulb connects to the amygdala via the piriform cortex of the primary olfactory cortex and directly projects from the main olfactory bulb to specific amygdala areas. The accessory olfactory bulb resides on the dorsal-posterior region of the main olfactory bulb and forms a parallel pathway. Destruction of the olfactory bulb results in ipsilateral anosmia, while irritative lesions of the uncus can result in olfactory and gustatory hallucinations.

The olfactory epithelium is a specialized epithelial tissue inside the nasal cavity that is involved in smell. In humans, it measures 5 cm2 (0.78 sq in) and lies on the roof of the nasal cavity about 7 cm (2.8 in) above and behind the nostrils. The olfactory epithelium is the part of the olfactory system directly responsible for detecting odors.

The glomerulus is a spherical structure located in the olfactory bulb of the brain where synapses form between the terminals of the olfactory nerve and the dendrites of mitral, periglomerular and tufted cells. Each glomerulus is surrounded by a heterogeneous population of juxtaglomerular neurons and glial cells.
Parosmia is a dysfunctional smell detection characterized by the inability of the brain to correctly identify an odor's "natural" smell. Instead, the natural odor is usually transformed into an unpleasant aroma, typically a "burned", "rotting", "fecal", or "chemical" smell. There can also be rare instances of a pleasant odor called euosmia. The condition was rare and little-researched until it became relatively more widespread since 2020 as a side effect of COVID-19.
In medicine and anatomy, the special senses are the senses that have specialized organs devoted to them:

The olfactory tubercle (OT), also known as the tuberculum olfactorium, is a multi-sensory processing center that is contained within the olfactory cortex and ventral striatum and plays a role in reward cognition. The OT has also been shown to play a role in locomotor and attentional behaviors, particularly in relation to social and sensory responsiveness, and it may be necessary for behavioral flexibility. The OT is interconnected with numerous brain regions, especially the sensory, arousal, and reward centers, thus making it a potentially critical interface between processing of sensory information and the subsequent behavioral responses.
Phantosmia, also called an olfactory hallucination or a phantom odor, is smelling an odor that is not actually there. This is intrinsically suspicious as the formal evaluation and detection of relatively low levels of odour particles is itself a very tricky task in air epistemology. It can occur in one nostril or both. Unpleasant phantosmia, cacosmia, is more common and is often described as smelling something that is burned, foul, spoiled, or rotten. Experiencing occasional phantom smells is normal and usually goes away on its own in time. When hallucinations of this type do not seem to go away or when they keep coming back, it can be very upsetting and can disrupt an individual's quality of life.
The primary olfactory cortex (POC) is a portion of the cerebral cortex. It is found in the inferior part of the temporal lobe of the brain. It receives input from the olfactory tract. It is involved in the sense of smell (olfaction).
Hyposmia, or microsmia, is a reduced ability to smell and to detect odors. A related condition is anosmia, in which no odors can be detected. Some of the causes of olfaction problems are allergies, nasal polyps, viral infections and head trauma. In 2012 an estimated 9.8 million people aged 40 and older in the United States had hyposmia and an additional 3.4 million had anosmia/severe hyposmia.
Olfactory fatigue, also known as odor fatigue, olfactory adaptation, and noseblindness, is the temporary, normal inability to distinguish a particular odor after a prolonged exposure to that airborne compound. For example, when entering a restaurant initially the odor of food is often perceived as being very strong, but after time the awareness of the odor normally fades to the point where the smell is not perceptible or is much weaker. After leaving the area of high odor, the sensitivity is restored with time. Anosmia is the permanent loss of the sense of smell, and is different from olfactory fatigue.
Dysosmia is a disorder described as any qualitative alteration or distortion of the perception of smell. Qualitative alterations differ from quantitative alterations, which include anosmia and hyposmia. Dysosmia can be classified as either parosmia or phantosmia. Parosmia is a distortion in the perception of an odorant. Odorants smell different from what one remembers. Phantosmia is the perception of an odor when no odorant is present. The cause of dysosmia still remains a theory. It is typically considered a neurological disorder and clinical associations with the disorder have been made. Most cases are described as idiopathic and the main antecedents related to parosmia are URTIs, head trauma, and nasal and paranasal sinus disease. Dysosmia tends to go away on its own but there are options for treatment for patients that want immediate relief.

The sense of smell, or olfaction, is the special sense through which smells are perceived. The sense of smell has many functions, including detecting desirable foods, hazards, and pheromones, and plays a role in taste.
Olfactory memory refers to the recollection of odors. Studies have found various characteristics of common memories of odor memory including persistence and high resistance to interference. Explicit memory is typically the form focused on in the studies of olfactory memory, though implicit forms of memory certainly supply distinct contributions to the understanding of odors and memories of them. Research has demonstrated that the changes to the olfactory bulb and main olfactory system following birth are extremely important and influential for maternal behavior. Mammalian olfactory cues play an important role in the coordination of the mother infant bond, and the following normal development of the offspring. Maternal breast odors are individually distinctive, and provide a basis for recognition of the mother by her offspring.

Sniffing is a perceptually-relevant behavior, defined as the active sampling of odors through the nasal cavity for the purpose of information acquisition. This behavior, displayed by all terrestrial vertebrates, is typically identified based upon changes in respiratory frequency and/or amplitude, and is often studied in the context of odor guided behaviors and olfactory perceptual tasks. Sniffing is quantified by measuring intra-nasal pressure or flow or air or, while less accurate, through a strain gauge on the chest to measure total respiratory volume. Strategies for sniffing behavior vary depending upon the animal, with small animals displaying sniffing frequencies ranging from 4 to 12 Hz but larger animals (humans) sniffing at much lower frequencies, usually less than 2 Hz. Subserving sniffing behaviors, evidence for an "olfactomotor" circuit in the brain exists, wherein perception or expectation of an odor can trigger brain respiratory center to allow for the modulation of sniffing frequency and amplitude and thus acquisition of odor information. Sniffing is analogous to other stimulus sampling behaviors, including visual saccades, active touch, and whisker movements in small animals. Atypical sniffing has been reported in cases of neurological disorders, especially those disorders characterized by impaired motor function and olfactory perception.
The University of Pennsylvania Smell Identification Test (UPSIT) is a test that is commercially available for smell identification to test the function of an individual's olfactory system.
Retronasal smell, retronasal olfaction, is the ability to perceive flavor dimensions of foods and drinks. Retronasal smell is a sensory modality that produces flavor. It is best described as a combination of traditional smell and taste modalities. Retronasal smell creates flavor from smell molecules in foods or drinks shunting up through the nasal passages as one is chewing. When people use the term "smell", they are usually referring to "orthonasal smell", or the perception of smell molecules that enter directly through the nose and up the nasal passages. Retronasal smell is critical for experiencing the flavor of foods and drinks. Flavor should be contrasted with taste, which refers to five specific dimensions: (1) sweet, (2) salty, (3) bitter, (4) sour, and (5) umami. Perceiving anything beyond these five dimensions, such as distinguishing the flavor of an apple from a pear for example, requires the sense of retronasal smell.

There is increasing evidence suggesting that COVID-19 causes both acute and chronic neurologicalor psychological symptoms. Caregivers of COVID-19 patients also show a higher than average prevalence of mental health concerns. These symptoms result from multiple different factors.
Smell training or olfactory training is the act of regularly sniffing or exposing oneself to robust aromas with the intention of regaining a sense of smell. The stimulating smells used are often selected from major smell categories, such as aromatic, flowery, fruity, and resinous. Using strong scents, the patient is asked to sniff each different smell for a minimum of 20 seconds, no less than two times per day, for three to six months or more. It is used as a rehabilitative therapy to help people who have anosmia or post-viral olfactory dysfunction, a symptom of COVID-19. It was considered a promising experimental treatment in a 2017 meta-analysis.