Pentamidine is an antimicrobial medication used to treat African trypanosomiasis, leishmaniasis, Balamuthia infections, babesiosis, and to prevent and treat pneumocystis pneumonia (PCP) in people with poor immune function. In African trypanosomiasis it is used for early disease before central nervous system involvement, as a second line option to suramin. It is an option for both visceral leishmaniasis and cutaneous leishmaniasis. Pentamidine can be given by injection into a vein or muscle or by inhalation.

A granuloma is an aggregation of macrophages that forms in response to chronic inflammation. This occurs when the immune system attempts to isolate foreign substances that it is otherwise unable to eliminate. Such substances include infectious organisms including bacteria and fungi, as well as other materials such as foreign objects, keratin, and suture fragments.

Cryptococcosis is a potentially fatal fungal infection of mainly the lungs, presenting as a pneumonia, and brain, where it appears as a meningitis. Cough, difficulty breathing, chest pain and fever are seen when the lungs are infected. When the brain is infected, symptoms include headache, fever, neck pain, nausea and vomiting, light sensitivity and confusion or changes in behavior. It can also affect other parts of the body including skin, where it may appear as several fluid-filled nodules with dead tissue.
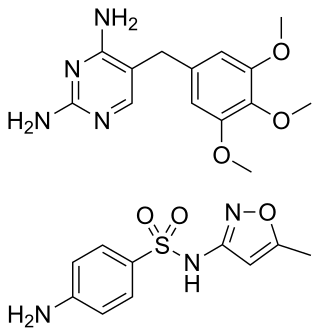
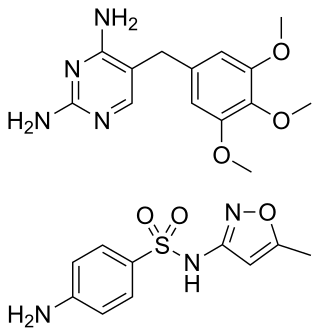
Trimethoprim/sulfamethoxazole, sold under the brand name Bactrim among others, is a fixed-dose combination antibiotic medication used to treat a variety of bacterial infections. It consists of one part trimethoprim to five parts sulfamethoxazole. It is used to treat urinary tract infections, methicillin-resistant Staphylococcus aureus (MRSA) skin infections, travelers' diarrhea, respiratory tract infections, and cholera, among others. It is used both to treat and prevent pneumocystis pneumonia and toxoplasmosis in people with HIV/AIDS and other causes of immunosuppression. It can be given orally or intravenous infusion.

Fungal infection, also known as mycosis, is a disease caused by fungi. Different types are traditionally divided according to the part of the body affected; superficial, subcutaneous, and systemic. Superficial fungal infections include common tinea of the skin, such as tinea of the body, groin, hands, feet and beard, and yeast infections such as pityriasis versicolor. Subcutaneous types include eumycetoma and chromoblastomycosis, which generally affect tissues in and beneath the skin. Systemic fungal infections are more serious and include cryptococcosis, histoplasmosis, pneumocystis pneumonia, aspergillosis and mucormycosis. Signs and symptoms range widely. There is usually a rash with superficial infection. Fungal infection within the skin or under the skin may present with a lump and skin changes. Pneumonia-like symptoms or meningitis may occur with a deeper or systemic infection.

Miliary tuberculosis is a form of tuberculosis that is characterized by a wide dissemination into the human body and by the tiny size of the lesions (1–5 mm). Its name comes from a distinctive pattern seen on a chest radiograph of many tiny spots distributed throughout the lung fields with the appearance similar to millet seeds—thus the term "miliary" tuberculosis. Miliary TB may infect any number of organs, including the lungs, liver, and spleen. Miliary tuberculosis is present in about 2% of all reported cases of tuberculosis and accounts for up to 20% of all extra-pulmonary tuberculosis cases.
AIDS-defining clinical conditions is the list of diseases published by the Centers for Disease Control and Prevention (CDC) that are associated with AIDS and used worldwide as a guideline for AIDS diagnosis. CDC exclusively uses the term AIDS-defining clinical conditions, but the other terms remain in common use.
WHO Disease Staging System for HIV Infection and Disease in Adults and Adolescents was first produced in 1990 by the World Health Organization and updated in September 2005. It is an approach for use in resource limited settings and is widely used in Africa and Asia and has been a useful research tool in studies of progression to symptomatic HIV disease.
The current staging system for HIV infection in children was developed in 2005 and builds upon the staging system in place since 1987. A child is defined as someone under the age of 15. This staging system also requires the presence of HIV infection: HIV antibody for children aged 18 months or more; virological or p24 antigen positive test if aged under 18 months.
The CDC Classification System for HIV Infection is the medical classification system used by the United States Centers for Disease Control and Prevention (CDC) to classify HIV disease and infection. The system is used to allow the government to handle epidemic statistics and define who receives US government assistance.
Talaromycosis is a fungal infection that presents with painless skin lesions of the face and neck, as well as an associated fever, anaemia, and enlargement of the lymph glands and liver.

Bacillary angiomatosis (BA) is a form of angiomatosis associated with bacteria of the genus Bartonella.

Paracoccidioidomycosis (PCM), also known as South American blastomycosis, is a fungal infection that can occur as a mouth and skin type, lymphangitic type, multi-organ involvement type (particularly lungs), or mixed type. If there are mouth ulcers or skin lesions, the disease is likely to be widespread. There may be no symptoms, or it may present with fever, sepsis, weight loss, large glands, or a large liver and spleen.

Pneumocystis pneumonia (PCP), also known as Pneumocystis jirovecii pneumonia (PJP), is a form of pneumonia that is caused by the yeast-like fungus Pneumocystis jirovecii.

Chronic multifocal Langerhans cell histiocytosis, previously known as Hand–Schüller–Christian disease, is a type of Langerhans cell histiocytosis (LCH), which can affect multiple organs. The condition is traditionally associated with a combination of three features; bulging eyes, breakdown of bone, and diabetes insipidus, although around 75% of cases do not have all three features. Other features may include a fever and weight loss, and depending on the organs involved there may be rashes, asymmetry of the face, ear infections, signs in the mouth and the appearance of advanced gum disease. Features relating to lung and liver disease may occur.
Diffuse infiltrative lymphocytosis syndrome (DILS) is a rare multi-system complication of HIV believed to occur secondary to an abnormal persistence of the initial CD8+ T cell expansion that regularly occurs in an HIV infection. This persistent CD8+ T cell expansion occurs in the setting of a low CD4+/CD8+ T cell ratio and ultimately invades and destroys tissues and organs resulting in the various complications of DILS. DILS classically presents with bilateral salivary gland enlargement (parotitis), cervical lymphadenopathy, and sicca symptoms such as xerophthalmia and xerostomia, but it may also involve the lungs, nervous system, kidneys, liver, digestive tract, and muscles. Once suspected, current diagnostic workups include (1) confirming HIV infection, (2) confirming six or greater months of characteristic signs and symptoms, (3) confirming organ infiltration by CD8+ T cells, and (4) exclusion of other autoimmune conditions. Once the diagnosis of DILS is confirmed, management includes highly active antiretroviral therapy (HAART) and as-needed steroids. With proper treatment, the overall prognosis of DILS is favorable.

Kaposi's sarcoma (KS) is a type of cancer that can form masses in the skin, in lymph nodes, in the mouth, or in other organs. The skin lesions are usually painless, purple and may be flat or raised. Lesions can occur singly, multiply in a limited area, or may be widespread. Depending on the sub-type of disease and level of immune suppression, KS may worsen either gradually or quickly. Except for Classical KS where there is generally no immune suppression, KS is caused by a combination of immune suppression and infection by Human herpesvirus 8.

The stages of HIV infection are acute infection, latency, and AIDS. Acute infection lasts for several weeks and may include symptoms such as fever, swollen lymph nodes, inflammation of the throat, rash, muscle pain, malaise, and mouth and esophageal sores. The latency stage involves few or no symptoms and can last anywhere from two weeks to twenty years or more, depending on the individual. AIDS, the final stage of HIV infection, is defined by low CD4+ T cell counts, various opportunistic infections, cancers, and other conditions.
Pneumocystis murina is a species of fungus, first isolated from laboratory mice, hence its name.. Pneumocystis murina is a species of fungi belonging to the genus Pneumocystis, characterized by its unique cyst-like multinucleate morphology and association with the respiratory tract of mammals. P. murina is particularly notable for its exclusive infection of laboratory mice and its role as an important model for studying human diseases, specifically Pneumocystis jirovecii infections in immunocompromised patients. Pneumocystis murina was first phylogenetically identified and described as a distinct species by Keely, S. P., Fischer, J. M., Cushion, M. T., and Stringer, J. R. in 2012.
Emmonsiosis, also known as emergomycosis, is a systemic fungal infection that can affect the lungs, generally always affects the skin and can become widespread. The lesions in the skin look like small red bumps and patches with a dip, ulcer and dead tissue in the centre.