Tramadol, sold under the brand name Ultram among others, is an opioid pain medication and a serotonin–norepinephrine reuptake inhibitor (SNRI) used to treat moderately severe pain. When taken by mouth in an immediate-release formulation, the onset of pain relief usually begins within an hour. It is also available by injection. It is available in combination with paracetamol (acetaminophen).

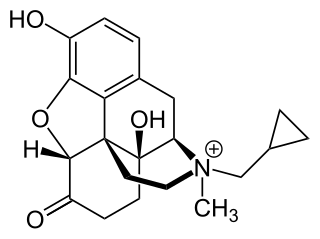
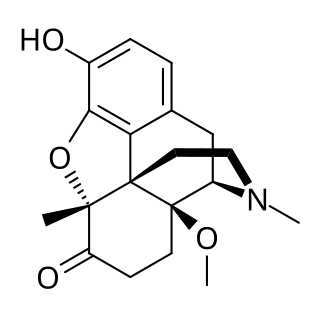
Hydromorphone, also known as dihydromorphinone, and sold under the brand name Dilaudid among others, is a morphinan opioid used to treat moderate to severe pain. Typically, long-term use is only recommended for pain due to cancer. It may be used by mouth or by injection into a vein, muscle, or under the skin. Effects generally begin within half an hour and last for up to five hours. A 2016 Cochrane review found little difference in benefit between hydromorphone and other opioids for cancer pain.

Sevoflurane, sold under the brand name Sevorane, among others, is a sweet-smelling, nonflammable, highly fluorinated methyl isopropyl ether used as an inhalational anaesthetic for induction and maintenance of general anesthesia. After desflurane, it is the volatile anesthetic with the fastest onset. While its offset may be faster than agents other than desflurane in a few circumstances, its offset is more often similar to that of the much older agent isoflurane. While sevoflurane is only half as soluble as isoflurane in blood, the tissue blood partition coefficients of isoflurane and sevoflurane are quite similar. For example, in the muscle group: isoflurane 2.62 vs. sevoflurane 2.57. In the fat group: isoflurane 52 vs. sevoflurane 50. As a result, the longer the case, the more similar will be the emergence times for sevoflurane and isoflurane.

Opioids are a class of drugs that derive from, or mimic, natural substances found in the opium poppy plant. Opioids work in the brain to produce a variety of effects, including pain relief. As a class of substances, they act on opioid receptors to produce morphine-like effects.

Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opiod into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true analgesia, motor, sensory and autonomic (sympathetic) blockade. Administering analgesics in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation, some autonomic blockade, but no sensory or motor block. Locoregional analgesia, due to mainly the absence of motor and sympathetic block may be preferred over locoregional anaesthesia in some postoperative care settings. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.

An anesthetic or anaesthetic is a drug used to induce anesthesia — in other words, to result in a temporary loss of sensation or awareness. They may be divided into two broad classes: general anesthetics, which result in a reversible loss of consciousness, and local anesthetics, which cause a reversible loss of sensation for a limited region of the body without necessarily affecting consciousness.

Epidural administration is a method of medication administration in which a medicine is injected into the epidural space around the spinal cord. The epidural route is used by physicians and nurse anesthetists to administer local anesthetic agents, analgesics, diagnostic medicines such as radiocontrast agents, and other medicines such as glucocorticoids. Epidural administration involves the placement of a catheter into the epidural space, which may remain in place for the duration of the treatment. The technique of intentional epidural administration of medication was first described in 1921 by Spanish military surgeon Fidel Pagés.

Remifentanil, marketed under the brand name Ultiva is a potent, short-acting synthetic opioid analgesic drug. It is given to patients during surgery to relieve pain and as an adjunct to an anaesthetic. Remifentanil is used for sedation as well as combined with other medications for use in general anesthesia. The use of remifentanil has made possible the use of high-dose opioid and low-dose hypnotic anesthesia, due to synergism between remifentanil and various hypnotic drugs and volatile anesthetics.

Intrathecal administration is a route of administration for drugs via an injection into the spinal canal, or into the subarachnoid space so that it reaches the cerebrospinal fluid (CSF). It is useful in several applications, such as for spinal anesthesia, chemotherapy, or pain management. This route is also used to introduce drugs that fight certain infections, particularly post-neurosurgical. Typically, the drug is given this way to avoid being stopped by the blood–brain barrier, as it may not be able to pass into the brain when given orally. Drugs given by the intrathecal route often have to be compounded specially by a pharmacist or technician because they cannot contain any preservative or other potentially harmful inactive ingredients that are sometimes found in standard injectable drug preparations.

Nalbuphine, sold under the brand names Nubain among others, is an opioid analgesic which is used in the treatment of pain. It is given by injection into a vein, muscle, or fat.

Piritramide(R-3365, trade names Dipidolor, Piridolan, Pirium and others) is a synthetic opioid analgesic that is marketed in certain European countries including: Austria, Belgium, Czech Republic, Slovenia, Germany and the Netherlands. It comes in free form, is about 0.75x times as potent as morphine and is given parenterally for the treatment of severe pain. Nausea, vomiting, respiratory depression and constipation are believed to be less frequent with piritramide than with morphine, and it produces more rapid-onset analgesia when compared to morphine and pethidine. After intravenous administration the onset of analgesia is as little as 1–2 minutes, which may be related to its great lipophilicity. The analgesic and sedative effects of piritramide are believed to be potentiated with phenothiazines and its emetic (nausea/vomiting-inducing) effects are suppressed. The volume of distribution is 0.7-1 L/kg after a single dose, 4.7-6 L/kg after steady-state concentrations are achieved and up to 11.1 L/kg after prolonged dosing.
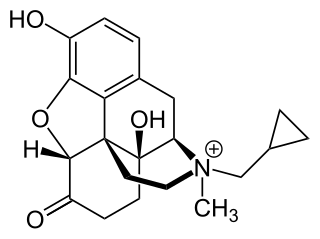
Methylnaltrexone, used in form of methylnaltrexone bromide, is a medication that acts as a peripherally acting μ-opioid receptor antagonist that acts to reverse some of the side effects of opioid drugs such as constipation without significantly affecting pain relief or precipitating withdrawals. Because MNTX is a quaternary ammonium cation, it cannot cross the blood–brain barrier, and so has antagonist effects throughout the body, counteracting effects such as itching and constipation, but without affecting opioid effects in the brain such as pain relief. However, since a significant fraction of opioid analgesia can be mediated by opioid receptors on peripheral sensory neurons, particularly in inflammatory conditions such as arthritis, traumatic or surgical pain, MNTX may increase pain under such circumstances.
Dezocine, sold under the brand name Dalgan, is an atypical opioid analgesic which is used in the treatment of pain. It is used by intravenous infusion and intramuscular injection.
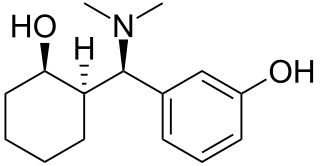
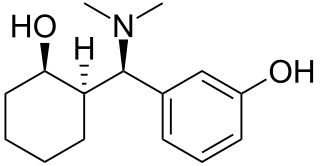
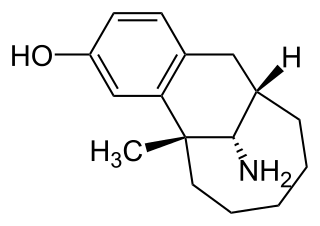
Ciramadol (WY-15,705) is an opioid analgesic that was developed in the late 1970s and is related to phencyclidine, tramadol, tapentadol and venlafaxine. It is a mixed agonist-antagonist for the μ-opioid receptor with relatively low abuse potential and a ceiling on respiratory depression which makes it a relatively safe drug. It has a slightly higher potency and effectiveness as an analgesic than codeine, but is weaker than morphine. Other side effects include sedation and nausea but these are generally less severe than with other similar drugs.
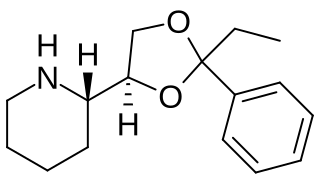
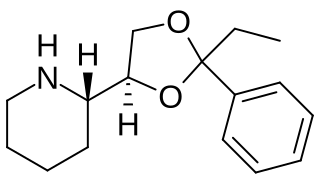
Etoxadrol (CL-1848C) is a dissociative anaesthetic drug that has been found to be an NMDA antagonist and produce similar effects to PCP in animals. Etoxadrol, along with another related drug dexoxadrol, were developed as analgesics for use in humans, but development was discontinued in the late 1970s after patients reported side effects such as nightmares and hallucinations.

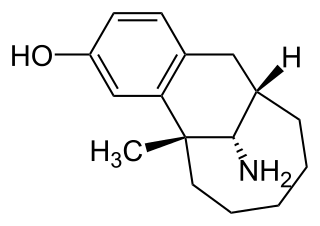
Levallorphan, also known as levallorphan tartrate (USAN), is an opioid modulator of the morphinan family used as an opioid analgesic and opioid antagonist/antidote. It acts as an antagonist of the μ-opioid receptor (MOR) and as an agonist of the κ-opioid receptor (KOR), and as a result, blocks the effects of stronger agents with greater intrinsic activity such as morphine whilst simultaneously producing analgesia.
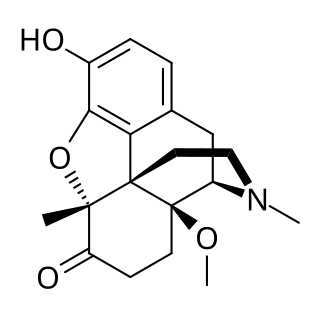
14-Methoxymetopon is an experimental opioid drug developed by a team led by Professor Helmut Schmidhammer at the University of Innsbruck in the mid-1990s. It is a derivative of metopon in which a methoxy group has been inserted at the 14-position. It is a highly potent analgesic drug that is around 500 times stronger than morphine when administered systemically; however, when given spinally or supraspinally, it exhibits analgesic activity up to a million fold greater than morphine. It binds strongly to the μ-opioid receptor and activates it to a greater extent than most similar opioid drugs. This produces an unusual pharmacological profile, and although 14-methoxymetopon acts as a potent μ-opioid full agonist in regard to some effects such as analgesia, a ceiling effect is seen on other effects such as constipation and respiratory depression which is believed to involve interaction with the κ-opioid receptor

Ocfentanil is a potent synthetic opioid structurally related to fentanyl that was developed in the early 1990s as one of a series of potent naloxone-reversible opioids in an attempt to obtain an opioid that had better therapeutic indices in terms of cardiovascular effects and respiratory depression as compared to fentanyl. Ocfentanil was never developed for medical use despite reasonable results in human clinical trials, but subsequently started to be sold as a designer drug starting in around 2013.

Pentamorphone is a semi-synthetic opiate derivative related to compounds such as Morphinone and oxymorphone. Developed in 1984, it is a potent opioid analgesic several times stronger than fentanyl, and with a similarly fast onset of effects and short duration of action. It was found to produce relatively little respiratory depression compared to other potent opioid agonists, but its analgesic effects were somewhat disappointing in human trials, and while pentamorphone had some slight advantages over fentanyl these were not sufficient to warrant its introduction into clinical use.

Frakefamide (INN) is a synthetic, fluorinated linear tetrapeptide with the amino acid sequence Tyr-D-Ala-(p-F)Phe-Phe-NH2 which acts as a peripherally-specific, selective μ-opioid receptor agonist. Despite its inability to penetrate the blood-brain-barrier and enter the central nervous system, frakefamide has potent analgesic effects and, unlike centrally-acting opioids like morphine, does not produce respiratory depression, indicating that its antinociceptive effects are mediated by peripheral μ-opioid receptors. It was under development for the treatment of pain by AstraZeneca and Shire but was shelved after phase II clinical trials.