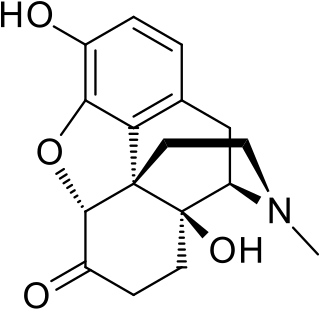
Hydromorphone, also known as dihydromorphinone, and sold under the brand name Dilaudid among others, is a morphinan opioid used to treat moderate to severe pain. Typically, long-term use is only recommended for pain due to cancer. It may be used by mouth or by injection into a vein, muscle, or under the skin. Effects generally begin within half an hour and last for up to five hours. A 2016 Cochrane review found little difference in benefit between hydromorphone and other opioids for cancer pain.

Opioids are a class of drugs that derive from, or mimic, natural substances found in the opium poppy plant. Opioids work in the brain to produce a variety of effects, including pain relief. As a class of substances, they act on opioid receptors to produce morphine-like effects.

Buprenorphine, sold under the brand name Subutex among others, is an opioid used to treat opioid use disorder, acute pain, and chronic pain. It can be used under the tongue (sublingual), in the cheek (buccal), by injection, as a skin patch (transdermal), or as an implant. For opioid use disorder, it is typically started when withdrawal symptoms have begun and for the first two days of treatment under direct observation of a health-care provider.
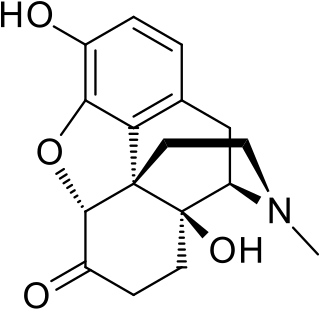
Oxymorphone is a highly potent opioid analgesic indicated for treatment of severe pain. Pain relief after injection begins after about 5–10 minutes, after oral administration it begins after about 30 minutes, and lasts about 3–4 hours for immediate-release tablets and 12 hours for extended-release tablets. The elimination half-life of oxymorphone is much faster intravenously, and as such, the drug is most commonly used orally. Like oxycodone, which metabolizes to oxymorphone, oxymorphone has a high potential to be abused.

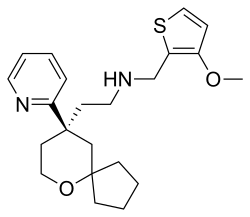
Sufentanil, sold under the brand names Dsuvia and Sufenta, is a synthetic opioid analgesic drug approximately 5 to 10 times as potent as its parent drug, fentanyl, and 500 times as potent as morphine. Structurally, sufentanil differs from fentanyl through the addition of a methoxymethyl group on the piperidine ring, and the replacement of the phenyl ring by thiophene. Sufentanil first was synthesized at Janssen Pharmaceutica in 1974.

Lubiprostone, sold under the brand name Amitiza among others, is a medication used in the management of chronic idiopathic constipation, predominantly irritable bowel syndrome-associated constipation in women and opioid-induced constipation. The drug is owned by Mallinckrodt and is marketed by Takeda Pharmaceutical Company.
Mepolizumab, sold under the brand name Nucala by GlaxoSmithKline, is a humanized monoclonal antibody used for the treatment of severe eosinophilic asthma, eosinophilic granulomatosis, and hypereosinophilic syndrome (HES). It recognizes and blocks interleukin-5 (IL-5), a signalling protein of the immune system.
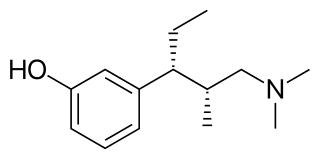
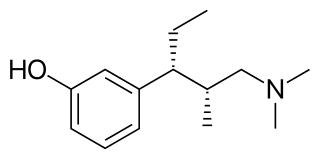
Tapentadol, brand names Nucynta among others, is a centrally acting opioid analgesic of the benzenoid class with a dual mode of action as an agonist of the μ-opioid receptor and as a norepinephrine reuptake inhibitor (NRI). Analgesia occurs within 32 minutes of oral administration, and lasts for 4–6 hours.

An opiate, is an alkaloid substance derived from opium It has a different meaning from the similar term opioid, used to designate all substances, both natural and synthetic, that bind to opioid receptors in the brain. Opiates are alkaloid compounds naturally found in the opium poppy plant Papaver somniferum. The psychoactive compounds found in the opium plant include morphine, codeine, and thebaine. Opiates have long been used for a variety of medical conditions with evidence of opiate trade and use for pain relief as early as the eighth century AD. Most opiates are considered drugs with moderate to high abuse potential and are listed on various "Substance-Control Schedules" under the Uniform Controlled Substances Act of the United States of America. Some, such as thebaine don't share the same effects and are not classified as controlled substances.
Trevena Inc is a clinical stage biopharmaceutical company, headquartered in Chesterbrook, Pennsylvania, USA, and is involved in the discovery and development of G-protein coupled receptors (GPCR) biased ligands. Trevena was founded in 2007 with technology licensed from Duke University, which originated in the labs of company founders Robert Lefkowitz winner of the 2012 Nobel Prize in Chemistry and Howard Rockman. Trevena's approach to drug discovery is based on utilizing ligand bias, or functional selectivity, at GPCR targets to produce drugs with improved efficacy and reduced side effect profiles. Trevena was named one of the top 15 US startups of 2008 by Business Week.
Ixekizumab, sold under the brand name Taltz, is an injectable medication for the treatment of autoimmune diseases. Chemically, it is a form of a humanized monoclonal antibody. The substance acts by binding interleukin 17A and neutralizing it, reducing inflammation.

Naldemedine is a medication that is used for the treatment of opioid-induced constipation in adults with chronic non-cancer pain. It is a peripherally acting μ-opioid receptor antagonist and was developed by Shionogi. Clinical studies have found it to possess statistically significant effectiveness for these indications and to be generally well tolerated, with predominantly mild to moderate gastrointestinal side effects. Effects indicative of central opioid withdrawal or impact on the analgesic or miotic effects of co-administered opioids have only been observed in a small number of patients.
Dupilumab, sold under the brand name Dupixent, is a monoclonal antibody blocking interleukin 4 and interleukin 13, used for allergic diseases such as eczema, asthma and nasal polyps which result in chronic sinusitis. It is also used for the treatment of eosinophilic esophagitis and prurigo nodularis.

Atezolizumab, sold under the brand name Tecentriq, is a monoclonal antibody medication used to treat urothelial carcinoma, non-small cell lung cancer (NSCLC), small cell lung cancer (SCLC), hepatocellular carcinoma and alveolar soft part sarcoma, but discontinued for use in triple-negative breast cancer (TNBC). It is a fully humanized, engineered monoclonal antibody of IgG1 isotype against the protein programmed cell death-ligand 1 (PD-L1).

Difelikefalin, sold under the brand name Korsuva, is an opioid peptide used for the treatment of moderate to severe itch. It acts as a peripherally-restricted, highly selective agonist of the κ-opioid receptor (KOR).
Risankizumab, sold under the brand name Skyrizi, is a humanized monoclonal antibody used for the treatment of plaque psoriasis, psoriatic arthritis, and Crohn's disease. It is designed to target interleukin 23A (IL-23A). It is given by subcutaneous injection.
Lanadelumab, sold under the brand name Takhzyro, is a human monoclonal antibody that targets plasma kallikrein (pKal) in order to promote prevention of angioedema in people with hereditary angioedema. Lanadelumab, was approved in the United States as the first monoclonal antibody indicated for prophylactic treatment to prevent hereditary angioedema attacks. Lanadelumab is the first treatment for hereditary angioedema prevention made by using cells within a lab, not human plasma.

Upadacitinib, sold under the brand name Rinvoq, is a medication used for the treatment of rheumatoid arthritis, psoriatic arthritis, atopic dermatitis, ulcerative colitis, Crohn's disease, ankylosing spondylitis, and axial spondyloarthritis. Upadacitinib is a Janus kinase (JAK) inhibitor that works by blocking the action of enzymes called Janus kinases. These enzymes are involved in setting up processes that lead to inflammation, and blocking their effect brings inflammation in the joints under control.
Satralizumab, sold under the brand name Enspryng, is a humanized monoclonal antibody medication that is used for the treatment of neuromyelitis optica spectrum disorder (NMOSD), a rare autoimmune disease. The drug is being developed by Chugai Pharmaceutical, a subsidiary of Roche.
Givosiran, sold under the brand name Givlaari, is a medication used for the treatment of adults with acute hepatic porphyria. Givosiran is a small interfering RNA (siRNA) directed towards delta-aminolevulinate synthase 1 (ALAS1), an important enzyme in the production of heme.