Related Research Articles

Leukemia is a group of blood cancers that usually begin in the bone marrow and result in high numbers of abnormal blood cells. These blood cells are not fully developed and are called blasts or leukemia cells. Symptoms may include bleeding and bruising, bone pain, fatigue, fever, and an increased risk of infections. These symptoms occur due to a lack of normal blood cells. Diagnosis is typically made by blood tests or bone marrow biopsy.

A myelodysplastic syndrome (MDS) is one of a group of cancers in which immature blood cells in the bone marrow do not mature, and as a result, do not develop into healthy blood cells. Early on, no symptoms typically are seen. Later, symptoms may include fatigue, shortness of breath, bleeding disorders, anemia, or frequent infections. Some types may develop into acute myeloid leukemia.

Fanconi anemia (FA) is a rare, autosomal recessive, genetic disease resulting in impaired response to DNA damage in the FA/BRCA pathway. Although it is a very rare disorder, study of this and other bone marrow failure syndromes has improved scientific understanding of the mechanisms of normal bone marrow function and development of cancer. Among those affected, the majority develop cancer, most often acute myelogenous leukemia (AML), MDS, and liver tumors. 90% develop aplastic anemia by age 40. About 60–75% have congenital defects, commonly short stature, abnormalities of the skin, arms, head, eyes, kidneys, and ears, and developmental disabilities. Around 75% have some form of endocrine problem, with varying degrees of severity. 60% of FA is FANC-A, 16q24.3, which has later onset bone marrow failure.
Tumors of the hematopoietic and lymphoid tissues or tumours of the haematopoietic and lymphoid tissues are tumors that affect the blood, bone marrow, lymph, and lymphatic system. Because these tissues are all intimately connected through both the circulatory system and the immune system, a disease affecting one will often affect the others as well, making aplasia, myeloproliferation and lymphoproliferation closely related and often overlapping problems. While uncommon in solid tumors, chromosomal translocations are a common cause of these diseases. This commonly leads to a different approach in diagnosis and treatment of hematological malignancies. Hematological malignancies are malignant neoplasms ("cancer"), and they are generally treated by specialists in hematology and/or oncology. In some centers "hematology/oncology" is a single subspecialty of internal medicine while in others they are considered separate divisions. Not all hematological disorders are malignant ("cancerous"); these other blood conditions may also be managed by a hematologist.
Acute lymphoblastic leukemia (ALL) is a cancer of the lymphoid line of blood cells characterized by the development of large numbers of immature lymphocytes. Symptoms may include feeling tired, pale skin color, fever, easy bleeding or bruising, enlarged lymph nodes, or bone pain. As an acute leukemia, ALL progresses rapidly and is typically fatal within weeks or months if left untreated.
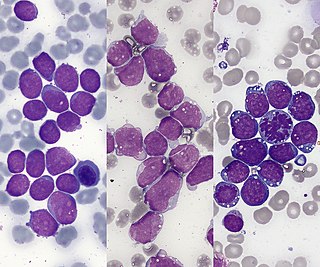
Acute promyelocytic leukemia is a subtype of acute myeloid leukemia (AML), a cancer of the white blood cells. In APL, there is an abnormal accumulation of immature granulocytes called promyelocytes. The disease is characterized by a chromosomal translocation involving the retinoic acid receptor alpha (RARA) gene and is distinguished from other forms of AML by its responsiveness to all-trans retinoic acid therapy. Acute promyelocytic leukemia was first characterized in 1957 by French and Norwegian physicians as a hyperacute fatal illness, with a median survival time of less than a week. Today, prognoses have drastically improved; 10-year survival rates are estimated to be approximately 80-90% according to one study.

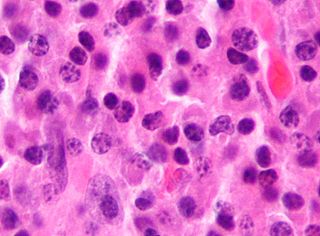
A myeloid sarcoma is a solid tumor composed of immature white blood cells called myeloblasts. A chloroma is an extramedullary manifestation of acute myeloid leukemia; in other words, it is a solid collection of leukemic cells occurring outside of the bone marrow.

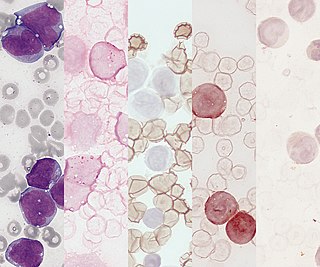
Acute erythrocyte leukemia is a rare form of acute myeloid leukemia where the myeloproliferation is of erythrocytic precursors. It is defined as type "M6" under the FAB classification.

Acute myeloid leukemia (AML) is a cancer of the myeloid line of blood cells, characterized by the rapid growth of abnormal cells that build up in the bone marrow and blood and interfere with normal blood cell production. Symptoms may include feeling tired, shortness of breath, easy bruising and bleeding, and increased risk of infection. Occasionally, spread may occur to the brain, skin, or gums. As an acute leukemia, AML progresses rapidly, and is typically fatal within weeks or months if left untreated.

A promyelocyte is a granulocyte precursor, developing from the myeloblast and developing into the myelocyte. Promyelocytes measure 12–20 microns in diameter. The nucleus of a promyelocyte is approximately the same size as a myeloblast but their cytoplasm is much more abundant. They also have less prominent nucleoli than myeloblasts and their chromatin is more coarse and clumped. The cytoplasm is basophilic and contains primary red/purple granules.
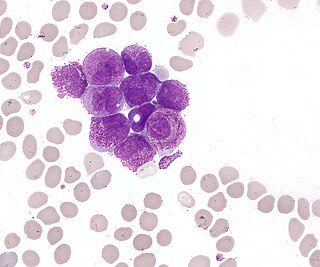
Acute monocytic leukemia is a type of acute myeloid leukemia. In AML-M5 >80% of the leukemic cells are of monocytic lineage. This cancer is characterized by a dominance of monocytes in the bone marrow. There is an overproduction of monocytes that the body does not need in the periphery. These overproduced monocytes interfere with normal immune cell production which causes many health complications for the affected individual.

Chronic myelomonocytic leukemia (CMML) is a type of leukemia, which are cancers of the blood-forming cells of the bone marrow. In adults, blood cells are formed in the bone marrow, by a process that is known as haematopoiesis. In CMML, there are increased numbers of monocytes and immature blood cells (blasts) in the peripheral blood and bone marrow, as well as abnormal looking cells (dysplasia) in at least one type of blood cell.

Acute myeloblastic leukemia with maturation (M2) is a subtype of acute myeloid leukemia (AML).
Juvenile myelomonocytic leukemia (JMML) is a rare form of chronic leukemia that affects children, commonly those aged four and younger. The name JMML now encompasses all diagnoses formerly referred to as juvenile chronic myeloid leukemia (JCML), chronic myelomonocytic leukemia of infancy, and infantile monosomy 7 syndrome. The average age of patients at diagnosis is two (2) years old. The World Health Organization has included JMML as a subcategory of myelodysplastic and myeloproliferative disorders.

Acute megakaryoblastic leukemia (AMKL) is life-threatening leukemia in which malignant megakaryoblasts proliferate abnormally and injure various tissues. Megakaryoblasts are the most immature precursor cells in a platelet-forming lineage; they mature to promegakaryocytes and, ultimately, megakaryocytes which cells shed membrane-enclosed particles, i.e. platelets, into the circulation. Platelets are critical for the normal clotting of blood. While malignant megakaryoblasts usually are the predominant proliferating and tissue-damaging cells, their similarly malignant descendants, promegakaryocytes and megakaryocytes, are variable contributors to the malignancy.

Blastic plasmacytoid dendritic cell neoplasm (BPDCN) is a rare hematologic malignancy. It was initially regarded as a form of lymphocyte-derived cutaneous lymphoma and alternatively named CD4+CD56+ hematodermic tumor, blastic NK cell lymphoma, and agranular CD4+ NK cell leukemia. Later, however, the disease was determined to be a malignancy of plasmacytoid dendritic cells rather than lymphocytes and therefore termed blastic plasmacytoid dendritic cell neoplasm. In 2016, the World Health Organization designated BPDCN to be in its own separate category within the myeloid class of neoplasms. It is estimated that BPDCN constitutes 0.44% of all hematological malignancies.

Childhood leukemia is leukemia that occurs in a child and is a type of childhood cancer. Childhood leukemia is the most common childhood cancer, accounting for 29% of cancers in children aged 0–14 in 2018. There are multiple forms of leukemia that occur in children, the most common being acute lymphoblastic leukemia (ALL) followed by acute myeloid leukemia (AML). Survival rates vary depending on the type of leukemia, but may be as high as 90% in ALL.
AI-10-49 is a small molecule inhibitor of leukemic oncoprotein CBFβ-SMHHC developed by the laboratory of John Bushweller with efficacy demonstrated by the laboratories of Lucio H. Castilla and Monica Guzman. AI-10-49 allosterically binds to CBFβ-SMMHC and disrupts protein-protein interaction between CBFβ-SMMHC and tumor suppressor RUNX1. This inhibitor is under development as an anti-leukemic drug.
Clonal hypereosinophilia, also termed primary hypereosinophilia or clonal eosinophilia, is a grouping of hematological disorders all of which are characterized by the development and growth of a pre-malignant or malignant population of eosinophils, a type of white blood cell that occupies the bone marrow, blood, and other tissues. This population consists of a clone of eosinophils, i.e. a group of genetically identical eosinophils derived from a sufficiently mutated ancestor cell.
GATA2 deficiency is a grouping of several disorders caused by common defect, namely, familial or sporadic inactivating mutations in one of the two parental GATA2 genes. Being the gene haploinsufficient, mutations that cause a reduction in the cellular levels of the gene's product, GATA2, are autosomal dominant. The GATA2 protein is a transcription factor critical for the embryonic development, maintenance, and functionality of blood-forming, lymphatic-forming, and other tissue-forming stem cells. In consequence of these mutations, cellular levels of GATA2 are deficient and individuals develop over time hematological, immunological, lymphatic, or other presentations that may begin as apparently benign abnormalities but commonly progress to severe organ failure, opportunistic infections, virus infection-induced cancers, the myelodysplastic syndrome, and/or leukemia. GATA2 deficiency is a life-threatening and precancerous condition.
References
- ↑ "Acute Myeloid Leukemia - Signs and Symptoms".
- 1 2 3 4 Seiter, Karen (2023-07-26). "Acute Myeloid Leukemia (AML): Practice Essentials, Pathophysiology, Etiology". Medscape Reference. Retrieved 2024-06-26.
- ↑ Yamamoto K, Nagata K, Tsurukubo Y, et al. (2002). "Translocation (8;12)(q13;p13) during disease progression in acute myelomonocytic leukemia with t(11;19)(q23;p13.1)". Cancer Genet. Cytogenet. 137 (1): 64–7. doi:10.1016/S0165-4608(02)00555-1. PMID 12377416.
- ↑ Zhang L, Alsabeh R, Mecucci C, et al. (2007). "Rare t(1;11)(q23;p15) in therapy-related myelodysplastic syndrome evolving into acute myelomonocytic leukemia: a case report and review of the literature". Cancer Genet. Cytogenet. 178 (1): 42–8. doi:10.1016/j.cancergencyto.2007.06.012. PMID 17889707.
- ↑ "Acute myelomonocytic leukemia | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Retrieved 2019-11-06.
- ↑ "Signs and Symptoms of Acute Myeloid Leukemia (AML)". www.cancer.org. Retrieved 2019-11-06.
- ↑ "Survival Rates for Chronic Myelomonocytic Leukemia". www.cancer.org. Retrieved 2019-11-06.
- ↑ "Acute Myeloid Leukemia". NORD (National Organization for Rare Disorders). Retrieved 2019-12-14.
- ↑ "Acute myelomonocytic leukemia (FAB AML M4)". www.pathologyoutlines.com. Retrieved 2019-11-06.
- ↑ "Acute Myeloid Leukemia (AML)". Cleveland Clinic. Retrieved 2019-11-06.
- 1 2 3 4 5 6 7 Verschuur, A. C. (2004, May). Acute myelomonocytic leukemia. Retrieved December 13, 2019, from https://www.orpha.net/data/patho/Pro/en/AcuteMyelomonocyticLeukemia-FRenPro8560.pdf.
- 1 2 "Chemotherapy for Acute Myeloid Leukemia (AML)". www.cancer.org. Retrieved 2019-11-06.
- ↑ "Acute Myeloid Leukemia (AML) Subtypes and Prognostic Factors". www.cancer.org. Retrieved 2019-12-14.
- ↑ Shirafuji, Naoki; Asano, Shigetaka; Kozai, Koji; Takahashi, Satoshi; Matsuda, Satoru; Takaku, Fumimaro; Nagata, Shigekazu (1988-01-01). "Production of granulocyte colony-stimulating factor by acute myelomonocytic leukemia cells". Leukemia Research. 12 (9): 745–750. doi:10.1016/0145-2126(88)90007-0. ISSN 0145-2126. PMID 2461497.