| Bankart lesion | |
|---|---|
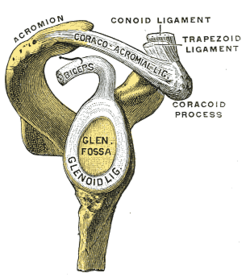 | |
| The glenoid labrum, labeled glenoid ligament, is damaged in a Bankart lesion. Lateral view demonstrating the articular surface of the right scapula is shown. | |
| Symptoms | Shoulder instability and widespread shoulder discomfort, and catching, locking, or popping feelings in shoulders. [1] |
| Risk factors | Anterior shoulder dislocation and/or repeated anterior shoulder subluxations. [2] |
| Diagnostic method | X-ray and MRI. |
| Differential diagnosis | Anterior labroligamentous periosteal sleeve avulsion, Rotator Cuff Tears, SLAP Lesion, Impingement, Perthes lesion, Glenolabral articular disruption, Humeral avulsion of the glenohumeral ligament. [2] |
A Bankart lesion is a type of shoulder injury that occurs following a dislocated shoulder. [3] It is an injury of the anterior (inferior) glenoid labrum of the shoulder. [4] When this happens, a pocket at the front of the glenoid forms that allows the humeral head to dislocate into it. It is an indication for surgery and often accompanied by a Hill–Sachs lesion, damage to the posterior humeral head. [5]
Contents
A bony Bankart is a Bankart lesion that includes a fracture of the anterior-inferior glenoid cavity of the scapula. [6]
The Bankart lesion is named after English orthopedic surgeon Arthur Sydney Blundell Bankart (1879–1951). [7]





