Related Research Articles

Bradycardia is a medical term used to describe a resting heart rate under 60 beats per minute (BPM). While bradycardia can result from a variety of pathologic processes, it is commonly a physiologic response to cardiovascular conditioning, or due to asymptomatic type 1 atrioventricular block. Resting heart rates less than 50 BPM are often normal during sleep in young and healthy adults, and in athletes. In large population studies of adults without underlying heart disease, resting heart rates of 45-50 BPM appear to be the lower limits of normal, dependent on age and sex. Bradycardia is most likely to be discovered in the elderly, as both age and underlying cardiac disease progression contribute to its development.

An artificial cardiac pacemaker is a medical device, nowadays always implanted, that generates electrical pulses delivered by electrodes to one or more of the chambers of the heart, the upper atria or lower ventricles. Each pulse causes the targeted chamber(s) to contract and pump blood, thus regulating the function of the electrical conduction system of the heart.

The contraction of cardiac muscle in all animals is initiated by electrical impulses known as action potentials that in the heart are known as cardiac action potentials. The rate at which these impulses fire controls the rate of cardiac contraction, that is, the heart rate. The cells that create these rhythmic impulses, setting the pace for blood pumping, are called pacemaker cells, and they directly control the heart rate. They make up the cardiac pacemaker, that is, the natural pacemaker of the heart. In most humans, the highest concentration of pacemaker cells is in the sinoatrial (SA) node, the natural and primary pacemaker, and the resultant rhythm is a sinus rhythm.

The Purkinje fibers are located in the inner ventricular walls of the heart, just beneath the endocardium in a space called the subendocardium. The Purkinje fibers are specialized conducting fibers composed of electrically excitable cells. They are larger than cardiomyocytes with fewer myofibrils and many mitochondria. They conduct cardiac action potentials more quickly and efficiently than any of the other cells in the heart's electrical conduction system. Purkinje fibers allow the heart's conduction system to create synchronized contractions of its ventricles, and are essential for maintaining a consistent heart rhythm.
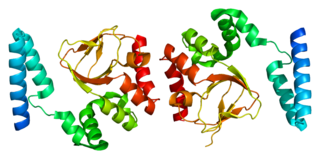
Atrial natriuretic peptide (ANP) or atrial natriuretic factor (ANF) is a natriuretic peptide hormone secreted from the cardiac atria that in humans is encoded by the NPPA gene. Natriuretic peptides are a family of hormone/paracrine factors that are structurally related. The main function of ANP is causing a reduction in expanded extracellular fluid (ECF) volume by increasing renal sodium excretion. ANP is synthesized and secreted by cardiac muscle cells in the walls of the atria in the heart. These cells contain volume receptors which respond to increased stretching of the atrial wall due to increased atrial blood volume.

The cardiac conduction system transmits the signals generated by the sinoatrial node – the heart's pacemaker, to cause the heart muscle to contract, and pump blood through the body's circulatory system. The pacemaking signal travels through the right atrium to the atrioventricular node, along the bundle of His, and through the bundle branches to Purkinje fibers in the walls of the ventricles. The Purkinje fibers transmit the signals more rapidly to stimulate contraction of the ventricles.

Cell therapy is a therapy in which viable cells are injected, grafted or implanted into a patient in order to effectuate a medicinal effect, for example, by transplanting T-cells capable of fighting cancer cells via cell-mediated immunity in the course of immunotherapy, or grafting stem cells to regenerate diseased tissues.

T-tubules are extensions of the cell membrane that penetrate into the center of skeletal and cardiac muscle cells. With membranes that contain large concentrations of ion channels, transporters, and pumps, T-tubules permit rapid transmission of the action potential into the cell, and also play an important role in regulating cellular calcium concentration.
Cardiomyoplasty is a surgical procedure in which healthy muscle from another part of the body is wrapped around the heart to provide support for the failing heart. Most often the latissimus dorsi muscle is used for this purpose. A special pacemaker is implanted to make the skeletal muscle contract. If cardiomyoplasty is successful and increased cardiac output is achieved, it usually acts as a bridging therapy, giving time for damaged myocardium to be treated in other ways, such as remodeling by cellular therapies.

Ryanodine receptor 2 (RYR2) is one of a class of ryanodine receptors and a protein found primarily in cardiac muscle. In humans, it is encoded by the RYR2 gene. In the process of cardiac calcium-induced calcium release, RYR2 is the major mediator for sarcoplasmic release of stored calcium ions.

Transcription factor GATA-4 is a protein that in humans is encoded by the GATA4 gene.

Potassium/sodium hyperpolarization-activated cyclic nucleotide-gated ion channel 2 is a protein that in humans is encoded by the HCN2 gene.

Atrial Light Chain-1 (ALC-1), also known as Essential Light Chain, Atrial is a protein that in humans is encoded by the MYL4 gene. ALC-1 is expressed in fetal cardiac ventricular and fetal skeletal muscle, as well as fetal and adult cardiac atrial tissue. ALC-1 expression is reactivated in human ventricular myocardium in various cardiac muscle diseases, including hypertrophic cardiomyopathy, dilated cardiomyopathy, ischemic cardiomyopathy and congenital heart diseases.
Potassium/sodium hyperpolarization-activated cyclic nucleotide-gated channel 4 is a protein that in humans is encoded by the HCN4 gene.

BRL-32872 is an experimental drug candidate that provides a novel approach to the treatment of cardiac arrhythmia. Being a derivative of verapamil, it possesses the ability to inhibit Ca+2 membrane channels. Specific modifications in hydrogen bonding activity, nitrogen lone pair availability, and molecular flexibility allow BRL-32872 to inhibit K+ channels as well. As such, BRL-32872 is classified as both a class III (K+ blocking) and class IV (Ca+2 blocking) antiarrhythmic agent.
Cardiac contractility modulation is a therapy which is intended for the treatment of patients with moderate to severe heart failure with symptoms despite optimal medical therapy who can benefit from an improvement in cardiac output. The short- and long-term use of this therapy enhances the strength of ventricular contraction and therefore the heart's pumping capacity by modulating (adjusting) the myocardial contractility. This is provided by a pacemaker-like device that applies non-excitatory electrical signals adjusted to and synchronized with the electrical action in the cardiac cycle.
Tbx18 transduction is a method of turning on genes in heart muscle cells as a treatment for certain cardiac arrhythmias. Currently this therapy is in the very early stages of experimentation, having only been applied to rodents. Before this treatment can be used in humans, successful tests on larger animals need to be completed followed by human clinical trials. This treatment is one of the many forms of gene therapy that are currently being researched for use in different diseases.
Human engineered cardiac tissues (hECTs) are derived by experimental manipulation of pluripotent stem cells, such as human embryonic stem cells (hESCs) and, more recently, human induced pluripotent stem cells (hiPSCs) to differentiate into human cardiomyocytes. Interest in these bioengineered cardiac tissues has risen due to their potential use in cardiovascular research and clinical therapies. These tissues provide a unique in vitro model to study cardiac physiology with a species-specific advantage over cultured animal cells in experimental studies. hECTs also have therapeutic potential for in vivo regeneration of heart muscle. hECTs provide a valuable resource to reproduce the normal development of human heart tissue, understand the development of human cardiovascular disease (CVD), and may lead to engineered tissue-based therapies for CVD patients.
Regeneration in humans is the regrowth of lost tissues or organs in response to injury. This is in contrast to wound healing, or partial regeneration, which involves closing up the injury site with some gradation of scar tissue. Some tissues such as skin, the vas deferens, and large organs including the liver can regrow quite readily, while others have been thought to have little or no capacity for regeneration following an injury.
References
- 1 2 3 Kenknight, B.; Girouard, S.D. (2013). "Chapter 3: Genetics - Patent Issued for Method for Controlling Pacemaker Therapy". In Acton, Q.A. (ed.). Arrhythmia: New Insights for the Healthcare Professional. Atlanta, GA: ScholarlyEditions. pp. 27–60. ISBN 9781481650717 . Retrieved 18 February 2016.
- 1 2 Ellis, Marie (17 July 2014). "Scientists create 'biological pacemakers' by transplanting gene into hearts". Medical News Today. MediLexicon International Ltd. Retrieved 18 February 2016.
- 1 2 Hattori, K. (22 June 2015). "Blue light sets the beat in biological pacemaker". Science Daily. Retrieved 18 February 2016.
- ↑ Ruhparwar, A.; Tebbenjohanns, J.; Niehaus, M.; et al. (2002). "Transplanted fetal cardiomyocytes as cardiac pacemaker". European Journal of Cardio-Thoracic Surgery. 21 (5): 853–857. doi: 10.1016/S1010-7940(02)00066-0 . PMID 12062274.
- ↑ Miake, J.; Marbán, E.; Nuss, H.B. (2002). "Biological pacemaker created by gene transfer". Nature. 419 (6903): 132–133. doi:10.1038/419132b. PMID 12226654. S2CID 4318994.
- ↑ Plotnikov, A.N.; Sosunov, E.A.; Qu, J.; et al. (2004). "Biological pacemaker implanted in canine left bundle branch provides ventricular escape rhythms that have physiologically acceptable rates". Circulation. 109 (4): 506–512. CiteSeerX 10.1.1.510.4284 . doi: 10.1161/01.CIR.0000114527.10764.CC . PMID 14734518.
- ↑ Ruhparwar, A.; Kallenbach, K.; Klein, G.; et al. (2010). "Adenylate-cyclase VI transforms ventricular cardiomyocytes into biological pacemaker cells". Tissue Engineering Part A. 16 (6): 1867–1872. doi:10.1089/ten.tea.2009.0537. PMID 20067385.