Related Research Articles

A sleep disorder, or somnipathy, is a medical disorder of an individual's sleep patterns. Some sleep disorders are severe enough to interfere with normal physical, mental, social and emotional functioning. Polysomnography and actigraphy are tests commonly ordered for diagnosing sleep disorders.
Dyssomnias are a broad classification of sleeping disorders involving difficulty getting to sleep, remaining asleep, or of excessive sleepiness.
Somnolence is a state of strong desire for sleep, or sleeping for unusually long periods. It has distinct meanings and causes. It can refer to the usual state preceding falling asleep, the condition of being in a drowsy state due to circadian rhythm disorders, or a symptom of other health problems. It can be accompanied by lethargy, weakness and lack of mental agility.
Hypersomnia is a neurological disorder of excessive time spent sleeping or excessive sleepiness. It can have many possible causes and can cause distress and problems with functioning. In the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), hypersomnolence, of which there are several subtypes, appears under sleep-wake disorders.
Sexsomnia, also known as sleep sex, is a distinct form of parasomnia, or an abnormal activity that occurs while an individual is asleep. Sexsomnia is characterized by an individual engaging in sexual acts while in non-rapid eye movement (NREM) sleep. Sexual behaviors that result from sexsomnia are not to be mistaken with normal nocturnal sexual behaviors, which do not occur during NREM sleep. Sexual behaviors that are viewed as normal during sleep and are accompanied by extensive research and documentation include nocturnal emissions, nocturnal erections, and sleep orgasms.
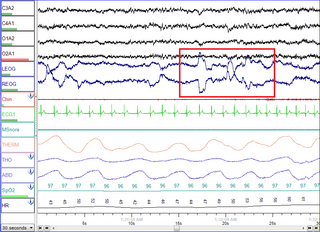
Polysomnography (PSG), a type of sleep study, is a multi-parameter study of sleep and a diagnostic tool in sleep medicine. The test result is called a polysomnogram, also abbreviated PSG. The name is derived from Greek and Latin roots: the Greek πολύς, the Latin somnus ("sleep"), and the Greek γράφειν.
Periodic limb movement disorder (PLMD) is a sleep disorder where the patient moves limbs involuntarily and periodically during sleep, and has symptoms or problems related to the movement. PLMD should not be confused with restless legs syndrome (RLS), which is characterized by a voluntary response to an urge to move legs due to discomfort. PLMD on the other hand is involuntary, and the patient is often unaware of these movements altogether. Periodic limb movements (PLMs) occurring during daytime period can be found but are considered as a symptom of RLS; only PLMs during sleep can suggest a diagnosis of PLMD.

Somnology is the scientific study of sleep. It includes clinical study and treatment of sleep disorders and irregularities. Sleep medicine is a subset of somnology.
Parasomnias are a category of sleep disorders that involve abnormal movements, behaviors, emotions, perceptions, and dreams that occur while falling asleep, sleeping, between sleep stages, or during arousal from sleep. Parasomnias are dissociated sleep states which are partial arousals during the transitions between wakefulness, NREM sleep, and REM sleep, and their combinations.
The International Classification of Sleep Disorders (ICSD) is "a primary diagnostic, epidemiological and coding resource for clinicians and researchers in the field of sleep and sleep medicine". The ICSD was produced by the American Academy of Sleep Medicine (AASM) in association with the European Sleep Research Society, the Japanese Society of Sleep Research, and the Latin American Sleep Society. The classification was developed as a revision and update of the Diagnostic Classification of Sleep and Arousal Disorders (DCSAD) that was produced by both the Association of Sleep Disorders Centers (ASDC) and the Association for the Psychophysiological Study of Sleep and was published in the journal Sleep in 1979. A second edition, called ICSD-2, was published by the AASM in 2005. The third edition, ICSD-3, was released by the AASM in 2014. A text revision of the third edition (ICSD-3-TR) was published in 2023 by the AASM.
When we sleep, our breathing changes due to normal biological processes that affect both our respiratory and muscular systems.

Sleep medicine is a medical specialty or subspecialty devoted to the diagnosis and therapy of sleep disturbances and disorders. From the middle of the 20th century, research has provided increasing knowledge of, and answered many questions about, sleep–wake functioning. The rapidly evolving field has become a recognized medical subspecialty in some countries. Dental sleep medicine also qualifies for board certification in some countries. Properly organized, minimum 12-month, postgraduate training programs are still being defined in the United States. In some countries, the sleep researchers and the physicians who treat patients may be the same people.

Catathrenia or nocturnal groaning is a sleep-related breathing disorder, consisting of end-inspiratory apnea and expiratory groaning during sleep. and it describes a rare condition characterized by monotonous, irregular groans while sleeping. Catathrenia begins with a deep inspiration. The person with catathrenia holds her or his breath against a closed glottis, similar to the Valsalva maneuver. Expiration can be slow and accompanied by sound caused by vibration of the vocal cords or a simple rapid exhalation. Despite a slower breathing rate, no oxygen desaturation usually occurs. The moaning sound is usually not noticed by the person producing the sound, but it can be extremely disturbing to sleep partners. It appears more often during expiration REM sleep than in NREM sleep.

A sleep study is a test that records the activity of the body during sleep. There are five main types of sleep studies that use different methods to test for different sleep characteristics and disorders. These include simple sleep studies, polysomnography, multiple sleep latency tests (MSLTs), maintenance of wakefulness tests (MWTs), and home sleep tests (HSTs). In medicine, sleep studies have been useful in identifying and ruling out various sleep disorders. Sleep studies have also been valuable to psychology, in which they have provided insight into brain activity and the other physiological factors of both sleep disorders and normal sleep. This has allowed further research to be done on the relationship between sleep and behavioral and psychological factors.

Narcolepsy is a chronic neurological disorder that involves a decreased ability to regulate sleep–wake cycles. Symptoms often include periods of excessive daytime sleepiness and brief involuntary sleep episodes. Narcolepsy paired with cataplexy is evidenced to be an autoimmune disorder. These experiences of cataplexy can be brought on by strong emotions. Less commonly, there may be vivid hallucinations or an inability to move while falling asleep or waking up. People with narcolepsy tend to sleep about the same number of hours per day as people without, but the quality of sleep tends to be lessened.
Idiopathic hypersomnia(IH) is a neurological disorder which is characterized primarily by excessive sleep and excessive daytime sleepiness (EDS). The condition typically becomes evident in early adulthood and most patients diagnosed with IH will have had the disorder for many years prior to their diagnosis. As of August 2021, an FDA-approved medication exists for IH called Xywav, which is oral solution of calcium, magnesium, potassium, and sodium oxybates; in addition to several off-label treatments (primarily FDA-approved narcolepsy medications).
Sleep disorder is a common repercussion of traumatic brain injury (TBI). It occurs in 30%-70% of patients with TBI. TBI can be distinguished into two categories, primary and secondary damage. Primary damage includes injuries of white matter, focal contusion, cerebral edema and hematomas, mostly occurring at the moment of the trauma. Secondary damage involves the damage of neurotransmitter release, inflammatory responses, mitochondrial dysfunctions and gene activation, occurring minutes to days following the trauma. Patients with sleeping disorders following TBI specifically develop insomnia, sleep apnea, narcolepsy, periodic limb movement disorder and hypersomnia. Furthermore, circadian sleep-wake disorders can occur after TBI.
Confusional arousals are classified as “partial awakenings in which the state of consciousness remains impaired for several minutes without any accompanying major behavioural disorders or severe autonomic responses”. Complete or partial amnesia of the episodes may be present.

Behavioral sleep medicine (BSM) is a field within sleep medicine that encompasses scientific inquiry and clinical treatment of sleep-related disorders, with a focus on the psychological, physiological, behavioral, cognitive, social, and cultural factors that affect sleep, as well as the impact of sleep on those factors. The clinical practice of BSM is an evidence-based behavioral health discipline that uses primarily non-pharmacological treatments. BSM interventions are typically problem-focused and oriented towards specific sleep complaints, but can be integrated with other medical or mental health treatments. The primary techniques used in BSM interventions involve education and systematic changes to the behaviors, thoughts, and environmental factors that initiate and maintain sleep-related difficulties.
References
- 1 2 3 Espie, Colin A; Morin, Charles M, eds. (2012). "Oxford Handbook of Sleep and Sleep Disorders - Oxford Handbooks". doi:10.1093/oxfordhb/9780195376203.001.0001. ISBN 9780195376203. Archived from the original on 2016-01-30. Retrieved 2016-03-12.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Chokroverty, Sudhansu; Billiard, Michel (2015-09-22). Sleep Medicine: A Comprehensive Guide to Its Development, Clinical Milestones, and Advances in Treatment. Springer. ISBN 9781493920891. Archived from the original on 2023-10-24. Retrieved 2023-10-24.
- ↑ Roger, H (1932). "Troubles du Sommeil". Masson et Cie, 1932; 275–83.
- ↑ Kleitman, N. (1939). Sleep and Wakefulness. Chicago: University of Chicago Press. pp. 280–9.
- ↑ Broughton, R. J. (1968-03-08). "Sleep disorders: disorders of arousal? Enuresis, somnambulism, and nightmares occur in confusional states of arousal, not in "dreaming sleep"". Science. 159 (3819): 1070–1078. doi:10.1126/science.159.3819.1070. ISSN 0036-8075. PMID 4865791. S2CID 11147846.
- ↑ Bickelmann, A. G.; Burwell, C. S.; Robin, E. D.; Whaley, R. D. (1956-11-01). "Extreme obesity associated with alveolar hypoventilation; a Pickwickian syndrome". The American Journal of Medicine. 21 (5): 811–818. doi:10.1016/0002-9343(56)90094-8. ISSN 0002-9343. PMID 13362309.
- ↑ Weitzman, E. D.; Czeisler, C. A.; Coleman, R. M.; Spielman, A. J.; Zimmerman, J. C.; Dement, W.; Richardson, G.; Pollak, C. P. (1981-07-01). "Delayed sleep phase syndrome. A chronobiological disorder with sleep-onset insomnia". Archives of General Psychiatry. 38 (7): 737–746. doi:10.1001/archpsyc.1981.01780320017001. ISSN 0003-990X. PMID 7247637.
- 1 2 "International Classification of Diseases, Revision 7 (1955)". www.wolfbane.com. Archived from the original on 2016-02-14. Retrieved 2016-03-11.
- 1 2 "International Classification of Diseases, Revision 8 (1965)". www.wolfbane.com. Archived from the original on 2016-03-06. Retrieved 2016-03-11.
- 1 2 "International Classification of Diseases, Revision 9 (1975)". www.wolfbane.com. Archived from the original on 2016-03-25. Retrieved 2016-03-11.
- ↑ "International Classification of Diseases, Revision 10 (1990)". www.wolfbane.com. Archived from the original on 2016-06-20. Retrieved 2016-03-11.
- ↑ "ICD-10-CM". Archived from the original on 2016-03-10. Retrieved 2016-03-11.
- ↑ "ICD11 Alpha : Morbidity". October 3, 2011. Archived from the original on 2011-10-03.
- ↑ Howard, P. Roffwarg (1979). "Diagnostic classification of sleep and arousal disorders. 1979 first edition. Association of Sleep Disorders Centers and the Association for the Psychophysiological Study of Sleep". Sleep. 2 (1): 1–154. doi: 10.1093/sleep/2.1.1 . PMID 531417.
- ↑ Thorpy, M. J. (1990-01-01). "Classification of sleep disorders". Journal of Clinical Neurophysiology. 7 (1): 67–81. doi:10.1097/00004691-199001000-00006. ISSN 0736-0258. PMC 3480567 . PMID 2406285.
- 1 2 THE INTERNATIONAL CLASSIFICATION OF SLEEP DISORDERS, REVISED Diagnostic and Coding Manual. Westchester, IL 60154-5767, U.S.A: American Academy of Sleep Medicine. 2001. ISBN 0-9657220-1-5.
{{cite book}}: CS1 maint: location (link) - ↑ American Academy of Sleep Medicine (2014). International Classification of Sleep Disorders - Third Edition. Darien, IL: American Academy of Sleep Medicine.
- ↑ "Application of the International Classification of Diseases to Neurology (ICD-NA) - WHO - OMS -". June 2, 2012. Archived from the original on 2012-06-02.
- ↑ "ICD-10-CM 2016". Archived from the original on 2016-03-10. Retrieved 2016-03-11.
- ↑ "ICD11 Alpha : Morbidity". October 3, 2011. Archived from the original on 2011-10-03.
- ↑ "Sleep Disorders" . DIAGNOSTIC AND STATISTICAL MANUAL OF MENTAL DISORDERS. WASHINGTON, DC, USA: AMERICAN PSYCHIATRIC ASSOCIATION. 2005. ISBN 0-89042-062-9.
- ↑ "DSM-5 Changes: Sleep-Wake Disorders". Psych Central.com. 7 June 2010. Archived from the original on 2016-03-02. Retrieved 2016-03-04.