Related Research Articles

Antipsychotics, previously known as neuroleptics and major tranquilizers, are a class of psychotropic medication primarily used to manage psychosis, principally in schizophrenia but also in a range of other psychotic disorders. They are also the mainstay, together with mood stabilizers, in the treatment of bipolar disorder. Moreover, they are also used as adjuncts in the treatment of treatment-resistant major depressive disorder.

Schizophrenia is a mental disorder characterized by hallucinations, delusions, disorganized thinking and behavior, and flat or inappropriate affect. Symptoms develop gradually and typically begin during young adulthood and are never resolved. There is no objective diagnostic test; diagnosis is based on observed behavior, a psychiatric history that includes the person's reported experiences, and reports of others familiar with the person. For a diagnosis of schizophrenia, the described symptoms need to have been present for at least six months or one month. Many people with schizophrenia have other mental disorders, especially mood disorders, anxiety disorders, and obsessive–compulsive disorder.

Dementia is a syndrome associated with many neurodegenerative diseases, characterized by a general decline in cognitive abilities that affects a person's ability to perform everyday activities. This typically involves problems with memory, thinking, behavior, and motor control. Aside from memory impairment and a disruption in thought patterns, the most common symptoms of dementia include emotional problems, difficulties with language, and decreased motivation. The symptoms may be described as occurring in a continuum over several stages. Dementia ultimately has a significant effect on the individual, their caregivers, and their social relationships in general. A diagnosis of dementia requires the observation of a change from a person's usual mental functioning and a greater cognitive decline than might be caused by the normal aging process.

Typical antipsychotics are a class of antipsychotic drugs first developed in the 1950s and used to treat psychosis. Typical antipsychotics may also be used for the treatment of acute mania, agitation, and other conditions. The first typical antipsychotics to come into medical use were the phenothiazines, namely chlorpromazine which was discovered serendipitously. Another prominent grouping of antipsychotics are the butyrophenones, an example of which is haloperidol. The newer, second-generation antipsychotics, also known as atypical antipsychotics, have largely supplanted the use of typical antipsychotics as first-line agents due to the higher risk of movement disorders with typical antipsychotics.

The atypical antipsychotics (AAP), also known as second generation antipsychotics (SGAs) and serotonin–dopamine antagonists (SDAs), are a group of antipsychotic drugs largely introduced after the 1970s and used to treat psychiatric conditions. Some atypical antipsychotics have received regulatory approval for schizophrenia, bipolar disorder, irritability in autism, and as an adjunct in major depressive disorder.

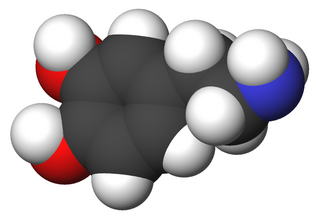
Quetiapine, sold under the brand name Seroquel among others, is an atypical antipsychotic medication used for the treatment of schizophrenia, bipolar disorder, and major depressive disorder. Despite being widely used as a sleep aid due to its sedating effect, the benefits of such use may not outweigh its undesirable side effects. It is taken orally.

Neurocognitive functions are cognitive functions closely linked to the function of particular areas, neural pathways, or cortical networks in the brain, ultimately served by the substrate of the brain's neurological matrix. Therefore, their understanding is closely linked to the practice of neuropsychology and cognitive neuroscience – two disciplines that broadly seek to understand how the structure and function of the brain relate to cognition and behaviour.
Tardive dyskinesia (TD) is an iatrogenic disorder that results in involuntary repetitive body movements, which may include grimacing, sticking out the tongue or smacking the lips, which occurs following treatment with medication. Additional motor symptoms include chorea or athetosis. In about 20% of people with TD, the disorder interferes with daily functioning. If TD is present in the setting of a long-term drug therapy, reversibility can be determined primarily by severity of symptoms and how long symptoms have been present before the long-term drug has been stopped.
Paraphrenia is a mental disorder characterized by an organized system of paranoid delusions with or without hallucinations and without deterioration of intellect or personality.
In medicine, a prodrome is an early sign or symptom that often indicates the onset of a disease before more diagnostically specific signs and symptoms develop. More specifically, it refers to the period between the first recognition of a disease's symptom until it reaches its more severe form. It is derived from the Greek word prodromos, meaning "running before". Prodromes may be non-specific symptoms or, in a few instances, may clearly indicate a particular disease, such as the prodromal migraine aura.
Geriatric psychiatry, also known as geropsychiatry, psychogeriatrics or psychiatry of old age, is a branch of medicine and a subspecialty of psychiatry dealing with the study, prevention, and treatment of neurodegenerative, cognitive impairment, and mental disorders in people of old age. Geriatric psychiatry as a subspecialty has significant overlap with the specialties of geriatric medicine, behavioural neurology, neuropsychiatry, neurology, and general psychiatry. Geriatric psychiatry has become an official subspecialty of psychiatry with a defined curriculum of study and core competencies.
Childhood schizophrenia is similar in characteristics of schizophrenia that develops at a later age, but has an onset before the age of 13 years, and is more difficult to diagnose. Schizophrenia is characterized by positive symptoms that can include hallucinations, delusions, and disorganized speech; negative symptoms, such as blunted affect and avolition and apathy, and a number of cognitive impairments. Differential diagnosis is problematic since several other neurodevelopmental disorders, including autism spectrum disorder, language disorder, and attention deficit hyperactivity disorder, also have signs and symptoms similar to childhood-onset schizophrenia.
The prognosis of schizophrenia is varied at the individual level. In general it has great human and economics costs. It results in a decreased life expectancy of 12–15 years primarily due to its association with obesity, little exercise, and smoking, while an increased rate of suicide plays a lesser role. These differences in life expectancy increased between the 1970s and 1990s, and between the 1990s and 2000s. This difference has not substantially changed in Finland for example – where there is a health system with open access to care.
The diagnosis of schizophrenia, a psychotic disorder, is based on criteria in either the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, or the World Health Organization's International Classification of Diseases (ICD). Clinical assessment of schizophrenia is carried out by a mental health professional based on observed behavior, reported experiences, and reports of others familiar with the person. Diagnosis is usually made by a psychiatrist. Associated symptoms occur along a continuum in the population and must reach a certain severity and level of impairment before a diagnosis is made. Schizophrenia has a prevalence rate of 0.3-0.7% in the United States.
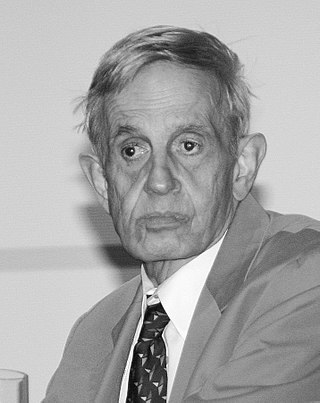
Perminder Sachdev is an Indian neuropsychiatrist based in Australia. He is a professor of neuropsychiatry at the University of New South Wales (UNSW), co-director of the UNSW Centre for Healthy Brain Aging, and clinical director of the Neuropsychiatric Institute at the Prince of Wales Hospital, Sydney. He is considered a trailblazer in the field of neuropsychiatry. Sachdev's research interests include ageing, vascular cognitive disorders such as vascular dementia, and psychiatric disorders.
Sam and Rose Stein Institute for Research on Aging is a non-profit, multidisciplinary research institute at the University of California, San Diego School of Medicine located in La Jolla, California. Established in 1983, it researches healthy aging through the development and application of the latest advances in biomedical and behavioral sciences.
The American Association for Geriatric Psychiatry is a learned society of professionals aiming to improve the quality of life for the elderly population, promote a healthy aging process, and a greater awareness of geriatric mental health issues.
Dopamine supersensitivity psychosis is a hypothesis that attempts to explain the phenomenon in which psychosis occurs despite treatment with escalating doses of antipsychotics. Dopamine supersensitivity may be caused by the dopamine receptor D2 antagonizing effect of antipsychotics, causing a compensatory increase in D2 receptors within the brain that sensitizes neurons to endogenous release of the neurotransmitter dopamine. Because psychosis is thought to be mediated—at least in part—by the activity of dopamine at D2 receptors, the activity of dopamine in the presence of supersensitivity may paradoxically give rise to worsening psychotic symptoms despite antipsychotic treatment at a given dose. This phenomenon may co-occur with tardive dyskinesia, a rare movement disorder that may also be due to dopamine supersensitivity.
The University of California, San Diego Performance-Based Skills Assessment (UPSA) was created by Dr. Thomas L. Patterson to provide a more reliable measure of every day functioning in patients with schizophrenia than the previously utilized methods such as self-report, clinician ratings or direct observation.
References
- 1 2 Jeste, Dilip V. (2020). Wiser: The Scientific Roots of Wisdom, Compassion, and What Makes Us Good. ISBN 978-1683644637.
- 1 2 "'Positive Psychiatry' Focus of New APA President's Term".
- 1 2 "PsychiatryOnline | Psychiatric News | News Article". pn.psychiatryonline.org. Archived from the original on 12 July 2012. Retrieved 27 January 2022.
- ↑ "Dilip Jeste - Institute of Medicine". Archived from the original on 2012-08-04. Retrieved 2011-08-31.
- ↑ "Focus on Asia at WCAP 2011". Archived from the original on 2011-10-31. Retrieved 2011-10-11.
- ↑ Seeking wisdom in graying matter, TEDMED, 2016-06-14, retrieved 2018-02-14
- ↑ http://hcr3.webofknowledge.com/author.cgi?&link1=Search&link2=Search%20Results&AuthLastName=Jeste&AuthFirstName=Dilip&AuthMiddleName=&AuthMailnstName=&CountryID=-1&DisciplineID=0&id=2594%5B%5D
- ↑ "NAMI | Pictures from 2012 Exemplary Psychiatrist Awards Ceremony". Archived from the original on 2013-10-05. Retrieved 2019-07-25.
- ↑ "Jeste Lab | UC San Diego Dept. Psychiatry".
- ↑ "International Psychogeriatric Association". Archived from the original on 2014-02-03. Retrieved 2012-10-22.
- ↑ "Home | Department of Psychiatry at UC San Diego School of Medicine". Archived from the original on November 20, 2011.
- ↑ "Wolters Kluwer Health".
- ↑ "International Psychogeriatrics". Cambridge Core. Retrieved 2018-02-14.
- ↑ Tarkan, Laurie (2008-06-24). "Doctors Say Medication Is Overused in Dementia". The New York Times.
- ↑ Rauch, Jonathan. "The Real Roots of Midlife Crisis". The Atlantic. Retrieved 2018-02-14.
- ↑ "The Times & the Sunday Times".[ dead link ]
- ↑ "Is wisdom in the brain?". Scientific American .
- ↑ Akitunde, Anthonia (2012-11-28). "Antipsychotic Drugs: 4 Commonly Used Meds Aren't Effective Or Safe For Older Adults, New Study Finds". The Huffington Post.
- ↑ http://www.medscape.com/viewarticle/511194 Secrets of Successful Aging: An Expert Interview With Dilip Jeste, MD
- ↑ http://jama.ama-assn.org/content/303/19/1980.full Successful Cognitive and Emotional Aging
- ↑ "Wisdom at the End of Life". UC Health - UC San Diego. Retrieved 2018-02-14.
- ↑ "Researchers Find Common Psychological Traits in Group of Italians Aged 90 to 101". UC Health - UC San Diego. Retrieved 2018-02-14.
- ↑ "Successful Dying: Researchers Define the Elements of a "Good Death"". UC Health - UC San Diego. Retrieved 2018-02-14.
- ↑ Neurobiology of Wisdom: A Literature Overview
- ↑ Expert Consensus on Characteristics of Wisdom: A Delphi Method Study
- ↑ Malaspina, Lauren; Woods, Steven Paul; Moore, David J.; Depp, Colin; Letendre, Scott L.; Jeste, Dilip; Grant, Igor; HIV Neurobehavioral Research Programs (HNRP) Group (Feb 2011). "Successful cognitive aging in persons living with HIV infection". J Neurovirol. 17 (1): 110–9. doi:10.1007/s13365-010-0008-z. PMC 3032198 . PMID 21165783.
- ↑ "Home | Department of Psychiatry at UC San Diego School of Medicine".
- ↑ "'Is there a doctor in the house?' There will be four at the Jeste Family residence in la Jolla! | la Jolla Light | la Jolla Light". Archived from the original on 2011-10-06. Retrieved 2011-08-31.