Related Research Articles

Shock is the state of insufficient blood flow to the tissues of the body as a result of problems with the circulatory system. Initial symptoms of shock may include weakness, fast heart rate, fast breathing, sweating, anxiety, and increased thirst. This may be followed by confusion, unconsciousness, or cardiac arrest, as complications worsen.

Sepsis is a potentially life-threatening condition that arises when the body's response to infection causes injury to its own tissues and organs.

Fluid replacement or fluid resuscitation is the medical practice of replenishing bodily fluid lost through sweating, bleeding, fluid shifts or other pathologic processes. Fluids can be replaced with oral rehydration therapy (drinking), intravenous therapy, rectally such as with a Murphy drip, or by hypodermoclysis, the direct injection of fluid into the subcutaneous tissue. Fluids administered by the oral and hypodermic routes are absorbed more slowly than those given intravenously.

Septic shock is a potentially fatal medical condition that occurs when sepsis, which is organ injury or damage in response to infection, leads to dangerously low blood pressure and abnormalities in cellular metabolism. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) defines septic shock as a subset of sepsis in which particularly profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk of mortality than with sepsis alone. Patients with septic shock can be clinically identified by requiring a vasopressor to maintain a mean arterial pressure of 65 mm Hg or greater and having serum lactate level greater than 2 mmol/L (>18 mg/dL) in the absence of hypovolemia. This combination is associated with hospital mortality rates greater than 40%.

Acute respiratory distress syndrome (ARDS) is a type of respiratory failure characterized by rapid onset of widespread inflammation in the lungs. Symptoms include shortness of breath (dyspnea), rapid breathing (tachypnea), and bluish skin coloration (cyanosis). For those who survive, a decreased quality of life is common.
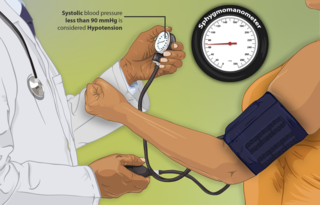
Hypotension, also known as low blood pressure, is a cardiovascular condition characterized by abnormally reduced blood pressure. Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps out blood and is indicated by two numbers, the systolic blood pressure and the diastolic blood pressure, which are the maximum and minimum blood pressures within the cardiac cycle, respectively. A systolic blood pressure of less than 90 millimeters of mercury (mmHg) or diastolic of less than 60 mmHg is generally considered to be hypotension. Different numbers apply to children. However, in practice, blood pressure is considered too low only if noticeable symptoms are present.

Hypovolemia, also known as volume depletion or volume contraction, is a state of abnormally low extracellular fluid in the body. This may be due to either a loss of both salt and water or a decrease in blood volume. Hypovolemia refers to the loss of extracellular fluid and should not be confused with dehydration.

Hypovolemic shock is a form of shock caused by severe hypovolemia. It could be the result of severe dehydration through a variety of mechanisms or blood loss. Hypovolemic shock is a medical emergency; if left untreated, the insufficient blood flow can cause damage to organs, leading to multiple organ failure.
Hyperchloremia is an electrolyte disturbance in which there is an elevated level of chloride ions in the blood. The normal serum range for chloride is 96 to 106 mEq/L, therefore chloride levels at or above 110 mEq/L usually indicate kidney dysfunction as it is a regulator of chloride concentration. As of now there are no specific symptoms of hyperchloremia; however, it can be influenced by multiple abnormalities that cause a loss of electrolyte-free fluid, loss of hypotonic fluid, or increased administration of sodium chloride. These abnormalities are caused by diarrhea, vomiting, increased sodium chloride intake, renal dysfunction, diuretic use, and diabetes. Hyperchloremia should not be mistaken for hyperchloremic metabolic acidosis as hyperchloremic metabolic acidosis is characterized by two major changes: a decrease in blood pH and bicarbonate levels, as well as an increase in blood chloride levels. Instead those with hyperchloremic metabolic acidosis are usually predisposed to hyperchloremia.

A pulmonary artery catheter (PAC), also known as a Swan-Ganz catheter or right heart catheter, is a balloon-tipped catheter that is inserted into a pulmonary artery in a procedure known as pulmonary artery catheterization or right heart catheterization. Pulmonary artery catheterization is a useful measure of the overall function of the heart particularly in those with complications from heart failure, heart attack, arrythmias or pulmonary embolism. It is also a good measure for those needing intravenous fluid therapy, for instance post heart surgery, shock, and severe burns. The procedure can also be used to measure pressures in the heart chambers.

Ringer's lactate solution (RL), also known as sodium lactate solution,Lactated Ringer's, and Hartmann's solution, is a mixture of sodium chloride, sodium lactate, potassium chloride, and calcium chloride in water. It is used for replacing fluids and electrolytes in those who have low blood volume or low blood pressure. It may also be used to treat metabolic acidosis and to wash the eye following a chemical burn. It is given by intravenous infusion or applied to the affected area.
Distributive shock is a medical condition in which abnormal distribution of blood flow in the smallest blood vessels results in inadequate supply of blood to the body's tissues and organs. It is one of four categories of shock, a condition where there is not enough oxygen-carrying blood to meet the metabolic needs of the cells which make up the body's tissues and organs. Distributive shock is different from the other three categories of shock in that it occurs even though the output of the heart is at or above a normal level. The most common cause is sepsis leading to a type of distributive shock called septic shock, a condition that can be fatal.
A post-anesthesia care unit (PACU) and sometimes referred to as post-anesthesia recovery or PAR, or simply recovery, is a part of hospitals, ambulatory care centers, and other medical facilities. Patients who received general anesthesia, regional anesthesia, or local anesthesia are transferred from the operating room suites to the recovery area. The patients are monitored typically by anesthesiologists, nurse anesthetists, and other medical staff. Providers follow a standardized handoff to the medical PACU staff that includes, which medications were given in the operating room suites, how hemodynamics were during the procedures, and what is expected for their recovery. After initial assessment and stabilization, patients are monitored for any potential complications, until the patient is transferred back to their hospital rooms.

Hydroxyethyl starch (HES/HAES), sold under the brand name Voluven among others, is a nonionic starch derivative, used as a volume expander in intravenous therapy. The use of HES on critically ill patients is associated with an increased risk of death and kidney problems.
The Surviving Sepsis Campaign (SSC) is a global initiative to bring together professional organizations in reducing mortality from sepsis. The purpose of the SSC is to create an international collaborative effort to improve the treatment of sepsis and reduce the high mortality rate associated with the condition. The Surviving Sepsis Campaign and the Institute for Healthcare Improvement have teamed up to achieve a 25 percent reduction in sepsis mortality by 2009. The guidelines were updated in 2016 and again in 2021.
A volume expander is a type of intravenous therapy that has the function of providing volume for the circulatory system. It may be used for fluid replacement or during surgery to prevent nausea and vomiting after surgery.
Emanuel Rivers is a physician born and raised in River Rouge, Michigan which is a suburb of Detroit, MI. He is board certified in emergency medicine, internal medicine and critical care medicine. Rivers has published extensively in the field of shock, sepsis and resuscitation.
The Sepsis Six is the name given to a bundle of medical therapies designed to reduce mortality in patients with sepsis.
quantium Medical Cardiac Output (qCO) uses impedance cardiography in a simple, continuous, and non-invasive way to estimate the cardiac output (CO) and other hemodynamic parameters such as the stroke volume (SV) and cardiac index (CI). The CO estimated by the qCO monitor is referred to as the "qCO". The impedance plethysmography allows determining changes in volume of the body tissues based on the measurement of the electric impedance at the body surface.

Vasopressin infusions are in use for septic shock patients not responding to fluid resuscitation or infusions of catecholamines to increase the blood pressure while sparing the use of catecholamines. These argipressins have much shorter elimination half-life than synthetic non-arginine vasopresines with much longer elimination half-life of many hours. Further, argipressins act on V1a, V1b, and V2 receptors which consequently lead to higher eGFR and lower vascular resistance in the lungs. A number of injectable arginine vasopressins are in clinical use in the United States and the European Union. Pitressin among others, is a medication most commonly used in the treatment of frequent urination, increased thirst, and dehydration such as that resulting from diabetes insipidus, which causes increased and diluted urine. It is used to treat abdominal distension following some surgeries, and in stomach roentgenography. Vasopressin is a hormone that affects the kidneys and reduces urine flow.
References
- ↑ Gordon, AC; Russell, JA (2005). "Goal directed therapy: How long can we wait?". Critical Care (Commentary). 9 (6): 647–8. doi: 10.1186/cc3951 . PMC 1414039 . PMID 16356258.
- ↑ Rossi, AF; Khan, DM; Hannan, R; Bolivar, J; et al. (January 2005). "Goal-directed medical therapy and point-of-care testing improve outcomes after congenital heart surgery". Intensive Care Medicine. 31 (1): 98–104. doi: 10.1007/s00134-004-2504-1 . PMID 15650863. S2CID 11746826.
- ↑ Rossi, AF; Khan, D (June 2004). "Point of care testing: Improving pediatric outcomes". Clinical Biochemistry. 37 (6): 456–61. doi:10.1016/j.clinbiochem.2004.04.004. PMID 15183294.
- ↑ Rivers, E; Nguyen, B; Havstad, S; Ressler, J; et al. (November 2001). "Early goal-directed therapy in the treatment of severe sepsis and septic shock". The New England Journal of Medicine . 345 (19): 1368–77. doi: 10.1056/NEJMoa010307 . PMID 11794169.
- 1 2 PRISM, Investigators.; Rowan, KM; Angus, DC; Bailey, M; Barnato, AE; Bellomo, R; Canter, RR; Coats, TJ; Delaney, A; Gimbel, E; Grieve, RD; Harrison, DA; Higgins, AM; Howe, B; Huang, DT; Kellum, JA; Mouncey, PR; Music, E; Peake, SL; Pike, F; Reade, MC; Sadique, MZ; Singer, M; Yealy, DM (8 June 2017). "Early, Goal-Directed Therapy for Septic Shock - A Patient-Level Meta-Analysis" (PDF). The New England Journal of Medicine. 376 (23): 2223–2234. doi: 10.1056/nejmoa1701380 . PMID 28320242.
- 1 2 3 4 5 6 7 Surviving Sepsis Campaign Guidelines Committee including The Pediatric Subgroup; Dellinger, R.P.; Levy, M.M.; Rhodes, A.; et al. (2013). "Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock: 2012" (PDF). Critical Care Medicine . 41 (2): 580–637. doi:10.1097/CCM.0b013e31827e83af. PMID 23353941. S2CID 34855187. Archived from the original (PDF) on 2015-02-02. Retrieved 2014-11-26– via Surviving Sepsis Campaign.
- ↑ Emergency Medicine Shock Research Network (EMShockNet), Investigators; Jones, AE; Shapiro, NI; Trzeciak, S; et al. (February 24, 2010). "Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: A randomized clinical trial". JAMA . 303 (8): 739–46. doi:10.1001/jama.2010.158. PMC 2918907 . PMID 20179283.