The brachiocephalic artery, brachiocephalic trunk, or innominate artery is an artery of the mediastinum that supplies blood to the right arm, head, and neck.

Aortic dissection (AD) occurs when an injury to the innermost layer of the aorta allows blood to flow between the layers of the aortic wall, forcing the layers apart. In most cases, this is associated with a sudden onset of severe chest or back pain, often described as "tearing" in character. Vomiting, sweating, and lightheadedness may also occur. Damage to other organs may result from the decreased blood supply, such as stroke, lower extremity ischemia, or mesenteric ischemia. Aortic dissection can quickly lead to death from insufficient blood flow to the heart or complete rupture of the aorta.
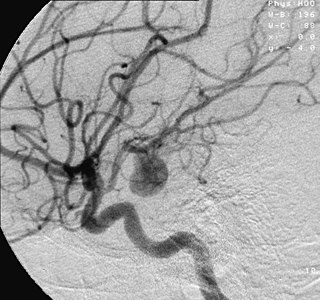
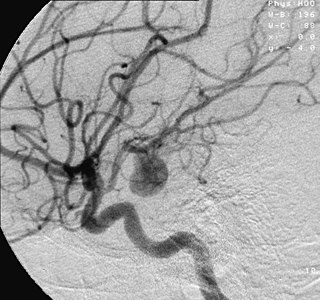
An aneurysm is an outward bulging, likened to a bubble or balloon, caused by a localized, abnormal, weak spot on a blood vessel wall. Aneurysms may be a result of a hereditary condition or an acquired disease. Aneurysms can also be a nidus for clot formation (thrombosis) and embolization. As an aneurysm increases in size, the risk of rupture, which leads to uncontrolled bleeding, increases. Although they may occur in any blood vessel, particularly lethal examples include aneurysms of the circle of Willis in the brain, aortic aneurysms affecting the thoracic aorta, and abdominal aortic aneurysms. Aneurysms can arise in the heart itself following a heart attack, including both ventricular and atrial septal aneurysms. There are congenital atrial septal aneurysms, a rare heart defect.

Vascular surgery is a surgical subspecialty in which vascular diseases involving the arteries, veins, or lymphatic vessels, are managed by medical therapy, minimally-invasive catheter procedures and surgical reconstruction. The specialty evolved from general and cardiovascular surgery where it refined the management of just the vessels, no longer treating the heart or other organs. Modern vascular surgery includes open surgery techniques, endovascular techniques and medical management of vascular diseases - unlike the parent specialities. The vascular surgeon is trained in the diagnosis and management of diseases affecting all parts of the vascular system excluding the coronaries and intracranial vasculature. Vascular surgeons also are called to assist other physicians to carry out surgery near vessels, or to salvage vascular injuries that include hemorrhage control, dissection, occlusion or simply for safe exposure of vascular structures.

An aortic aneurysm is an enlargement (dilatation) of the aorta to greater than 1.5 times normal size. They usually cause no symptoms except when ruptured. Occasionally, there may be abdominal, back, or leg pain. The prevalence of abdominal aortic aneurysm ("AAA") has been reported to range from 2 to 12% and is found in about 8% of men more than 65 years of age. The mortality rate attributable to AAA is about 15,000 per year in the United States and 6,000 to 8,000 per year in the United Kingdom and Ireland. Between 2001 and 2006, there were approximately 230,000 AAA surgical repairs performed on Medicare patients in the United States.
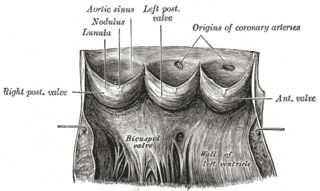
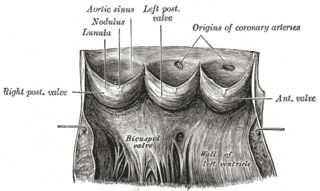
Aneurysm of the aortic sinus, also known as the sinus of Valsalva, is a rare abnormality of the aorta, the largest artery in the body. The aorta normally has three small pouches that sit directly above the aortic valve, and an aneurysm of one of these sinuses is a thin-walled swelling. Aneurysms may affect the right (65–85%), non-coronary (10–30%), or rarely the left coronary sinus. These aneurysms may not cause any symptoms but if large can cause shortness of breath, palpitations or blackouts. Aortic sinus aneurysms can burst or rupture into adjacent cardiac chambers, which can lead to heart failure if untreated.

Abdominal aortic aneurysm (AAA) is a localized enlargement of the abdominal aorta such that the diameter is greater than 3 cm or more than 50% larger than normal. An AAA usually causes no symptoms, except during rupture. Occasionally, abdominal, back, or leg pain may occur. Large aneurysms can sometimes be felt by pushing on the abdomen. Rupture may result in pain in the abdomen or back, low blood pressure, or loss of consciousness, and often results in death.

A thoracic aortic aneurysm is an aortic aneurysm that presents primarily in the thorax.
Aortic valve replacement is a procedure whereby the failing aortic valve of a patient's heart is replaced with an artificial heart valve. The aortic valve may need to be replaced because:
Interrupted aortic arch is a very rare heart defect in which the aorta is not completely developed. There is a gap between the ascending and descending thoracic aorta. In a sense it is the complete form of a coarctation of the aorta. Almost all patients also have other cardiac anomalies, including a ventricular septal defect (VSD), aorto-pulmonary window, and truncus arteriosus. There are three types of interrupted aortic arch, with type B being the most common. Interrupted aortic arch is often associated with DiGeorge syndrome.

Annuloaortic ectasia is characterized by pure aortic valve regurgitation and aneurysmal dilatation of the ascending aorta. Men are more likely than women to develop idiopathic annuloaortic ectasia, which usually manifests in the fourth or sixth decades of life. Additional factors that contribute to this condition include osteogenesis imperfecta, inflammatory aortic diseases, intrinsic valve disease, Loeys-Dietz syndrome, Marfan syndrome, and operated congenital heart disease.

Traumatic aortic rupture, also called traumatic aortic disruption or transection, is a condition in which the aorta, the largest artery in the body, is torn or ruptured as a result of trauma to the body. The condition is frequently fatal due to the profuse bleeding that results from the rupture. Since the aorta branches directly from the heart to supply blood to the rest of the body, the pressure within it is very great, and blood may be pumped out of a tear in the blood vessel very rapidly. This can quickly result in shock and death. Thus traumatic aortic rupture is a common killer in automotive accidents and other traumas, with up to 18% of deaths that occur in automobile collisions being related to the injury. In fact, aortic disruption due to blunt chest trauma is the second leading cause of injury death behind traumatic brain injury.

Endovascular aneurysm repair (EVAR) is a type of minimally-invasive endovascular surgery used to treat pathology of the aorta, most commonly an abdominal aortic aneurysm (AAA). When used to treat thoracic aortic disease, the procedure is then specifically termed TEVAR for "thoracic endovascular aortic/aneurysm repair." EVAR involves the placement of an expandable stent graft within the aorta to treat aortic disease without operating directly on the aorta. In 2003, EVAR surpassed open aortic surgery as the most common technique for repair of AAA, and in 2010, EVAR accounted for 78% of all intact AAA repair in the United States.

Randall Bertram Griepp was an American cardiothoracic surgeon who collaborated with Norman Shumway in the development of the first successful heart transplant procedures in the U.S. He had an international reputation for contributions to the surgical treatment of aortic aneurysms and aortic dissection and in heart and lung transplantations. He received nearly $8 million in grants from the National Heart, Lung, and Blood Institute.

A hybrid cardiac surgical procedure in a narrow sense is defined as a procedure that combines a conventional, more invasive surgical part with an interventional part, using some sort of catheter-based procedure guided by fluoroscopy imaging in a hybrid operating room (OR) without interruption. The hybrid technique has a reduced risk of surgical complications and has shown decreased recovery time. It can be used to treat numerous heart diseases and conditions and with the increasing complexity of each case, the hybrid surgical technique is becoming more common.

Open aortic surgery (OAS), also known as open aortic repair (OAR), describes a technique whereby an abdominal, thoracic or retroperitoneal surgical incision is used to visualize and control the aorta for purposes of treatment, usually by the replacement of the affected segment with a prosthetic graft. OAS is used to treat aneurysms of the abdominal and thoracic aorta, aortic dissection, acute aortic syndrome, and aortic ruptures. Aortobifemoral bypass is also used to treat atherosclerotic disease of the abdominal aorta below the level of the renal arteries. In 2003, OAS was surpassed by endovascular aneurysm repair (EVAR) as the most common technique for repairing abdominal aortic aneurysms in the United States.

Charles Granville Rob was a British surgeon who pioneered techniques in the repair of damaged blood vessels, particularly the operation to unblock arteries of the neck, known as carotid endarterectomy and of the aorta when treating aortic aneurysms.
Gustavo S. Oderich is a Brazilian American vascular and endovascular surgeon who serves as a professor and chief of vascular and endovascular surgery, and is the director of the Advanced Endovascular Aortic Program at McGovern Medical School at The University of Texas Health Science Center at Houston and Memorial Hermann Health System. He previously served as chair of vascular and endovascular division at the Mayo Clinic in Rochester, Minnesota. Oderich is recognized for his work in minimally invasive endovascular surgery and research in fenestrated and branched stent-graft technology to treat complex aortic aneurysms and dissections.
Spinal cord stroke is a rare type of stroke with compromised blood flow to any region of spinal cord owing to occlusion or bleeding, leading to irreversible neuronal death. It can be classified into two types, ischaemia and haemorrhage, in which the former accounts for 86% of all cases, a pattern similar to cerebral stroke. The disease is either arisen spontaneously from aortic illnesses or postoperatively. It deprives patients of motor function or sensory function, and sometimes both. Infarction usually occurs in regions perfused by anterior spinal artery, which spans the anterior two-thirds of spinal cord. Preventions of the disease include decreasing the risk factors and maintaining enough spinal cord perfusion pressure during and after the operation. The process of diagnosing the ischemic and hemorrhagic spinal cord stroke includes applying different MRI protocols and CT scan. Treatments for spinal cord stroke are mainly determined by the symptoms and the causes of the disease. For example, antiplatelet and corticosteroids might be used to reduce the risk of blood clots in ischaemic spinal stroke patients, while rapid surgical decompression is applied to minimize neurological injuries in haemorrhagic spinal stroke patients instead. Patients may spend years for rehabilitation after the spinal cord stroke.
Joseph S. Coselli is an American cardiothoracic surgeon who was the 96th president of the American Association for Thoracic Surgery (AATS), succeeding Pedro J. del Nido and preceding Thoralf M. Sundt, III. Coselli is a Professor and Executive Vice Chair in the Department of Surgery and the Cullen Foundation Endowed Chair at the Baylor College of Medicine.