Abortion is the termination of a pregnancy by removal or expulsion of an embryo or fetus. An abortion that occurs without intervention is known as a miscarriage or "spontaneous abortion"; these occur in approximately 30% to 40% of all pregnancies. When deliberate steps are taken to end a pregnancy, it is called an induced abortion, or less frequently "induced miscarriage". The unmodified word abortion generally refers to an induced abortion. The most common reasons women give for having an abortion are for birth-timing and limiting family size. Other reasons reported include maternal health, an inability to afford a child, domestic violence, lack of support, feeling they are too young, wishing to complete education or advance a career, and not being able or willing to raise a child conceived as a result of rape or incest.
Dilationand curettage (D&C) refers to the dilation of the cervix and surgical removal of sections and/or layers of the lining of the uterus and or contents of the uterus such as an unwanted fetus, remains of a non-viable fetus, retained placenta after birth or abortion as well as any abnormal tissue which may be in the uterus causing abnormal cycles by scraping and scooping (curettage). It is a gynecologic procedure used for treatment and removal as well as diagnostic and therapeutic purposes, and is the most commonly used method for first trimester abortion or miscarriage.
Intact dilation and extraction is a surgical procedure that terminates and removes an intact fetus from the uterus. The procedure is used both after miscarriages and for abortions in the second and third trimesters of pregnancy. When used to perform an abortion, an intact D&E can occur after feticide or on a live fetus.

Ectopic pregnancy is a complication of pregnancy in which the embryo attaches outside the uterus. Signs and symptoms classically include abdominal pain and vaginal bleeding, but fewer than 50 percent of affected women have both of these symptoms. The pain may be described as sharp, dull, or crampy. Pain may also spread to the shoulder if bleeding into the abdomen has occurred. Severe bleeding may result in a fast heart rate, fainting, or shock. With very rare exceptions, the fetus is unable to survive.
Late termination of pregnancy, also referred to politically as third trimester abortion, describes the termination of pregnancy by inducing labor during a late stage of gestation. In this context, late is not precisely defined, and different medical publications use varying gestational age thresholds. As of 2015, in the United States, more than 90% of abortions occur before the 13th week, 1.3% take place after the 21st week, and less than 1% occur after 24 weeks.

Selective reduction is the practice of reducing the number of fetuses in a multiple pregnancy, such as quadruplets, to a twin or singleton pregnancy. The procedure is also called multifetal pregnancy reduction. The procedure is most commonly done to reduce the number of fetuses in a multiple pregnancy to a safe number, when the multiple pregnancy is the result of use of assisted reproductive technology; outcomes for both the mother and the babies are generally worse the higher the number of fetuses. The procedure is also used in multiple pregnancies when one of the fetuses has a serious and incurable disease, or in the case where one of the fetuses is outside the uterus, in which case it is called selective termination.

Placenta praevia is when the placenta attaches inside the uterus but in a position near or over the cervical opening. Symptoms include vaginal bleeding in the second half of pregnancy. The bleeding is bright red and tends not to be associated with pain. Complications may include placenta accreta, dangerously low blood pressure, or bleeding after delivery. Complications for the baby may include fetal growth restriction.
A hysterotomy is an incision made in the uterus. This surgical incision is used in several medical procedures, including during termination of pregnancy in the second trimester and delivering the fetus during caesarean section. It is also used to gain access and perform surgery on a fetus during pregnancy to correct birth defects, and it is an option to achieve resuscitation if cardiac arrest occurs during pregnancy and it is necessary to remove the fetus from the uterus.
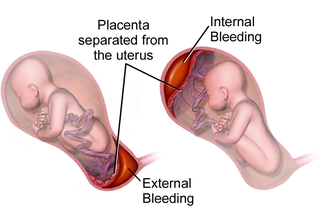
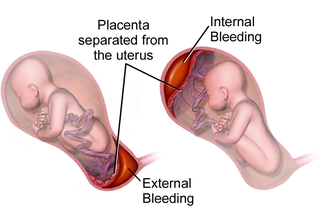
Placental abruption is when the placenta separates early from the uterus, in other words separates before childbirth. It occurs most commonly around 25 weeks of pregnancy. Symptoms may include vaginal bleeding, lower abdominal pain, and dangerously low blood pressure. Complications for the mother can include disseminated intravascular coagulopathy and kidney failure. Complications for the baby can include fetal distress, low birthweight, preterm delivery, and stillbirth.

Vacuum or suction aspiration is a procedure that uses a vacuum source to remove an embryo or fetus through the cervix. The procedure is performed to induce abortion, as a treatment for incomplete spontaneous abortion or retained fetal and placental tissue, or to obtain a sample of uterine lining. It is generally safe, and serious complications rarely occur.
Dilation and evacuation (D&E) or dilatation and evacuation is the dilation of the cervix and surgical evacuation of the uterus after the first trimester of pregnancy. It is a method of abortion as well as a common procedure used after miscarriage to remove all pregnancy tissue.

Complications of pregnancy are health problems that are related to, or arise during pregnancy. Complications that occur primarily during childbirth are termed obstetric labor complications, and problems that occur primarily after childbirth are termed puerperal disorders. While some complications improve or are fully resolved after pregnancy, some may lead to lasting effects, morbidity, or in the most severe cases, maternal or fetal mortality.

Placenta accreta occurs when all or part of the placenta attaches abnormally to the myometrium. Three grades of abnormal placental attachment are defined according to the depth of attachment and invasion into the muscular layers of the uterus:
- Accreta – chorionic villi attached to the myometrium, rather than being restricted within the decidua basalis.
- Increta – chorionic villi invaded into the myometrium.
- Percreta – chorionic villi invaded through the perimetrium.

Fetal surgery, also known as antenatal surgery or prenatal surgery, is a growing branch of maternal-fetal medicine that covers any of a broad range of surgical techniques that are used to treat congenital abnormalities in fetuses who are still in the pregnant uterus. There are three main types: open fetal surgery, which involves completely opening the uterus to operate on the fetus; minimally invasive fetoscopic surgery, which uses small incisions and is guided by fetoscopy and sonography; and percutaneous fetal therapy, which involves placing a catheter under continuous ultrasound guidance.

Uterine atony is the failure of the uterus to contract adequately following delivery. Contraction of the uterine muscles during labor compresses the blood vessels and slows flow, which helps prevent hemorrhage and facilitates coagulation. Therefore, a lack of uterine muscle contraction can lead to an acute hemorrhage, as the vasculature is not being sufficiently compressed. Uterine atony is the most common cause of postpartum hemorrhage, which is an emergency and potential cause of fatality. Across the globe, postpartum hemorrhage is among the top five causes of maternal death. Recognition of the warning signs of uterine atony in the setting of extensive postpartum bleeding should initiate interventions aimed at regaining stable uterine contraction.

A bicornuate uterus or bicornate uterus, is a type of Müllerian anomaly in the human uterus, where there is a deep indentation at the fundus (top) of the uterus.
Instillation abortion is a rarely used method of late-term abortion, performed by injecting a solution into the uterus.
Amnioinfusion is a method in which isotonic fluid is instilled into the uterine cavity.
Septic abortion describes any type of abortion, due to an upper genital tract bacterial infection including the inflammation of the endometrium during or after 20 weeks of gestation. The genital tract during this period is particularly vulnerable to infection, and sepsis in most cases is caused by a combination of factors both due to facility conditions and/or individual predispositions. The infection often starts in the placenta and fetus, with a potential complication of also affecting the uterus, that can result in sepsis spreading to surrounding organs, or pelvic infections.
A medical abortion, also known as medication abortion or non-surgical abortion, occurs when drugs (medication) are used to bring about an abortion. Medical abortions are an alternative to surgical abortions such as vacuum aspiration or dilation and curettage. Medical abortions are more common than surgical abortions in most places around the world.