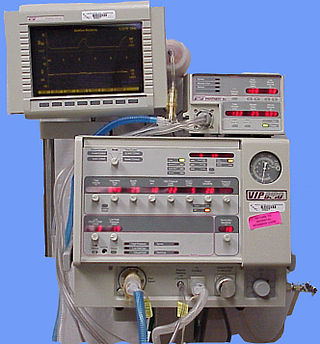
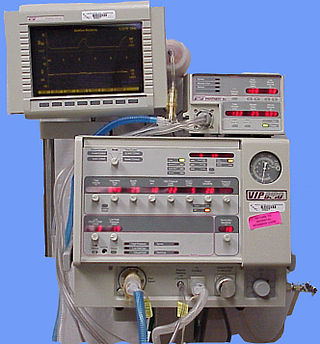
A ventilator is a type of breathing apparatus, a class of medical technology that provides mechanical ventilation by moving breathable air into and out of the lungs, to deliver breaths to a patient who is physically unable to breathe, or breathing insufficiently. Ventilators may be computerized microprocessor-controlled machines, but patients can also be ventilated with a simple, hand-operated bag valve mask. Ventilators are chiefly used in intensive-care medicine, home care, and emergency medicine and in anesthesiology.

Mechanical ventilation, assisted ventilation or intermittent mandatory ventilation (IMV) is the medical term for using a machine called a ventilator to fully or partially provide artificial ventilation. Mechanical ventilation helps move air into and out of the lungs, with the main goal of helping the delivery of oxygen and removal of carbon dioxide. Mechanical ventilation is used for many reasons, including to protect the airway due to mechanical or neurologic cause, to ensure adequate oxygenation, or to remove excess carbon dioxide from the lungs. Various healthcare providers are involved with the use of mechanical ventilation and people who require ventilators are typically monitored in an intensive care unit.

Tidal volume is the volume of air moved into or out of the lungs during a normal breath. In a healthy, young human adult, tidal volume is approximately 500 ml per inspiration or 7 ml/kg of body mass.

An iron lung is a type of negative pressure ventilator (NPV), a mechanical respirator which encloses most of a person's body, and varies the air pressure in the enclosed space, to stimulate breathing. It assists breathing when muscle control is lost, or the work of breathing exceeds the person's ability. Need for this treatment may result from diseases including polio and botulism and certain poisons.

Pulmonary edema, also known as pulmonary congestion, is excessive liquid accumulation in the tissue and air spaces of the lungs. It leads to impaired gas exchange and may cause hypoxemia and respiratory failure. It is due to either failure of the left ventricle of the heart to remove oxygenated blood adequately from the pulmonary circulation, or an injury to the lung tissue directly or blood vessels of the lung.

Acute respiratory distress syndrome (ARDS) is a type of respiratory failure characterized by rapid onset of widespread inflammation in the lungs. Symptoms include shortness of breath (dyspnea), rapid breathing (tachypnea), and bluish skin coloration (cyanosis). For those who survive, a decreased quality of life is common.

A bag valve mask (BVM), sometimes known by the proprietary name Ambu bag or generically as a manual resuscitator or "self-inflating bag", is a hand-held device commonly used to provide positive pressure ventilation to patients who are not breathing or not breathing adequately. The device is a required part of resuscitation kits for trained professionals in out-of-hospital settings (such as ambulance crews) and is also frequently used in hospitals as part of standard equipment found on a crash cart, in emergency rooms or other critical care settings. Underscoring the frequency and prominence of BVM use in the United States, the American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiac Care recommend that "all healthcare providers should be familiar with the use of the bag-mask device." Manual resuscitators are also used within the hospital for temporary ventilation of patients dependent on mechanical ventilators when the mechanical ventilator needs to be examined for possible malfunction or when ventilator-dependent patients are transported within the hospital. Two principal types of manual resuscitators exist; one version is self-filling with air, although additional oxygen (O2) can be added but is not necessary for the device to function. The other principal type of manual resuscitator (flow-inflation) is heavily used in non-emergency applications in the operating room to ventilate patients during anesthesia induction and recovery.
Ventilator-associated pneumonia (VAP) is a type of lung infection that occurs in people who are on mechanical ventilation breathing machines in hospitals. As such, VAP typically affects critically ill persons that are in an intensive care unit (ICU) and have been on a mechanical ventilator for at least 48 hours. VAP is a major source of increased illness and death. Persons with VAP have increased lengths of ICU hospitalization and have up to a 20–30% death rate. The diagnosis of VAP varies among hospitals and providers but usually requires a new infiltrate on chest x-ray plus two or more other factors. These factors include temperatures of >38 °C or <36 °C, a white blood cell count of >12 × 109/ml, purulent secretions from the airways in the lung, and/or reduction in gas exchange.
Positive end-expiratory pressure (PEEP) is the pressure in the lungs above atmospheric pressure that exists at the end of expiration. The two types of PEEP are extrinsic PEEP and intrinsic PEEP. Pressure that is applied or increased during an inspiration is termed pressure support.PEEP is a therapeutic parameter set in the ventilator, or a complication of mechanical ventilation with air trapping (auto-PEEP).
High-frequency ventilation is a type of mechanical ventilation which utilizes a respiratory rate greater than four times the normal value. and very small tidal volumes. High frequency ventilation is thought to reduce ventilator-associated lung injury (VALI), especially in the context of ARDS and acute lung injury. This is commonly referred to as lung protective ventilation. There are different types of high-frequency ventilation. Each type has its own unique advantages and disadvantages. The types of HFV are characterized by the delivery system and the type of exhalation phase.
Ventilator-associated lung injury (VALI) is an acute lung injury that develops during mechanical ventilation and is termed ventilator-induced lung injury (VILI) if it can be proven that the mechanical ventilation caused the acute lung injury. In contrast, ventilator-associated lung injury (VALI) exists if the cause cannot be proven. VALI is the appropriate term in most situations because it is virtually impossible to prove what actually caused the lung injury in the hospital.
Neurally adjusted ventilatory assist (NAVA) is a mode of mechanical ventilation. NAVA delivers assistance in proportion to and in synchrony with the patient's respiratory efforts, as reflected by an electrical signal. This signal represents the electrical activity of the diaphragm, the body's principal breathing muscle.

Airway pressure release ventilation (APRV) is a pressure control mode of mechanical ventilation that utilizes an inverse ratio ventilation strategy. APRV is an applied continuous positive airway pressure (CPAP) that at a set timed interval releases the applied pressure. Depending on the ventilator manufacturer, it may be referred to as BiVent. This is just as appropriate to use, since the only difference is that the term APRV is copyrighted.
Modes of mechanical ventilation are one of the most important aspects of the usage of mechanical ventilation. The mode refers to the method of inspiratory support. In general, mode selection is based on clinician familiarity and institutional preferences, since there is a paucity of evidence indicating that the mode affects clinical outcome. The most frequently used forms of volume-limited mechanical ventilation are intermittent mandatory ventilation (IMV) and continuous mandatory ventilation (CMV). There have been substantial changes in the nomenclature of mechanical ventilation over the years, but more recently it has become standardized by many respirology and pulmonology groups. Writing a mode is most proper in all capital letters with a dash between the control variable and the strategy.
Continuous mandatory ventilation (CMV) is a mode of mechanical ventilation in which breaths are delivered based on set variables. Still used in the operating room, in previous nomenclature, CMV referred to "controlled mechanical ventilation", a mode of ventilation characterized by a ventilator that makes no effort to sense patient breathing effort. In continuous mandatory ventilation, the ventilator can be triggered either by the patient or mechanically by the ventilator. The ventilator is set to deliver a breath according to parameters selected by the operator. "Controlled mechanical ventilation" is an outdated expansion for "CMV"; "continuous mandatory ventilation" is now accepted standard nomenclature for mechanical ventilation. CMV today can assist or control itself dynamically, depending on the transient presence or absence of spontaneous breathing effort. Thus, today's CMV would have been called ACV in older nomenclature, and the original form of CMV is a thing of the past. But despite continual technological improvement over the past half century, CMV may still be uncomfortable for the patient.
Intermittent Mandatory Ventilation (IMV) refers to any mode of mechanical ventilation where a regular series of breaths are scheduled but the ventilator senses patient effort and reschedules mandatory breaths based on the calculated need of the patient. Similar to continuous mandatory ventilation in parameters set for the patients pressures and volumes but distinct in its ability to support a patient by either supporting their own effort or providing support when patient effort is not sensed. IMV is frequently paired with additional strategies to improve weaning from ventilator support or to improve cardiovascular stability in patients who may need full life support.
Prone ventilation, sometimes called prone positioning or proning, refers to mechanical ventilation with the patient lying face-down (prone). It improves oxygenation in most patients with acute respiratory distress syndrome (ARDS) and reduces mortality. The earliest trial investigating the benefits of prone ventilation occurred in 1976. Since that time, many meta-analyses and one randomized control trial, the PROSEVA trial, have shown an increase in patients' survival with the more severe versions of ARDS. There are many proposed mechanisms, but they are not fully delineated. The proposed utility of prone ventilation is that this position will improve lung mechanics, improve oxygenation, and increase survival. Although improved oxygenation has been shown in multiple studies, this position change's survival benefit is not as clear. Similar to the slow adoption of low tidal volume ventilation utilized in ARDS, many believe that the investigation into the benefits of prone ventilation will likely be ongoing in the future.
Rheotrauma is a medical term for the harm caused to a patient's lungs by high gas flows as delivered by mechanical ventilation. Although mechanical ventilation may prevent death of a patient from the hypoxia or hypercarbia which may be caused by respiratory failure, it can also be damaging to the lungs, leading to ventilator-associated lung injury. Rheotrauma is one of the ways in which mechanical ventilation may do this, alongside volutrauma, barotrauma, atelectotrauma and biotrauma. Attempts have been made to combine all of the mechanical forces caused by the ventilator on the patient's lungs in an all encompassing term: mechanical power.
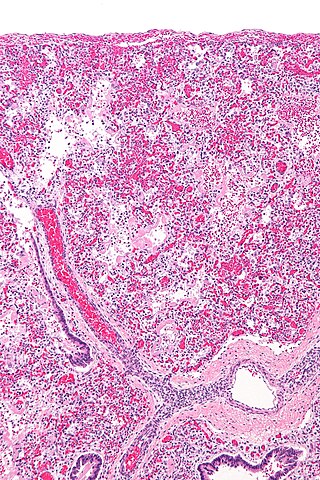
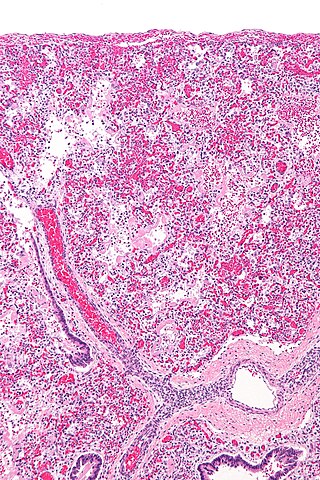
The pathophysiology of acute respiratory distress syndrome involves fluid accumulation in the lungs not explained by heart failure. It is typically provoked by an acute injury to the lungs that results in flooding of the lungs' microscopic air sacs responsible for the exchange of gases such as oxygen and carbon dioxide with capillaries in the lungs. Additional common findings in ARDS include partial collapse of the lungs (atelectasis) and low levels of oxygen in the blood (hypoxemia). The clinical syndrome is associated with pathological findings including pneumonia, eosinophilic pneumonia, cryptogenic organizing pneumonia, acute fibrinous organizing pneumonia, and diffuse alveolar damage (DAD). Of these, the pathology most commonly associated with ARDS is DAD, which is characterized by a diffuse inflammation of lung tissue. The triggering insult to the tissue usually results in an initial release of chemical signals and other inflammatory mediators secreted by local epithelial and endothelial cells.

Proning or prone positioning is the placement of patients into a prone position so that they are lying on their front. This is used in the treatment of patients in intensive care with acute respiratory distress syndrome (ARDS). It has been especially tried and studied for patients on ventilators but, during the COVID-19 pandemic, it is being used for patients with oxygen masks and CPAP as an alternative to ventilation.
There is no agreed upon equation for Mechanical Power.