Neisseria gonorrhoeae, also known as gonococcus (singular), or gonococci (plural), is a species of Gram-negative diplococci bacteria isolated by Albert Neisser in 1879. It causes the sexually transmitted genitourinary infection gonorrhea as well as other forms of gonococcal disease including disseminated gonococcemia, septic arthritis, and gonococcal ophthalmia neonatorum.

Neisseria is a large genus of bacteria that colonize the mucosal surfaces of many animals. Of the 11 species that colonize humans, only two are pathogens, N. meningitidis and N. gonorrhoeae. Most gonococcal infections are asymptomatic and self-resolving, and epidemic strains of the meningococcus may be carried in >95% of a population where systemic disease occurs at <1% prevalence.

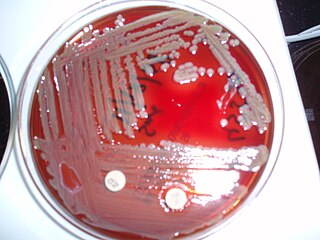
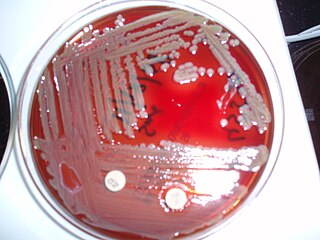
An agar plate is a Petri dish that contains a growth medium solidified with agar, used to culture microorganisms. Sometimes selective compounds are added to influence growth, such as antibiotics.
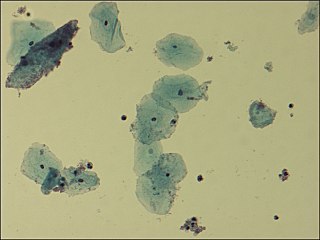
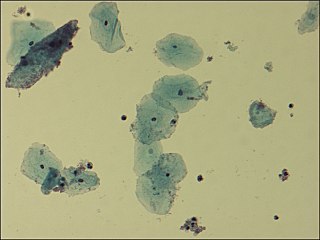
Gardnerella is a genus of Gram-variable-staining facultative anaerobic bacteria of which Gardnerella vaginalis is the only species. The organisms are small non-spore-forming, nonmotile coccobacilli.

Cryptococcus, sometimes informally called crypto, is a genus of fungi that grow in culture as yeasts. The sexual forms or teleomorphs of Cryptococcus species are filamentous fungi formerly classified in the genus Filobasidiella. The name Cryptococcus is used when referring to the yeast states of the fungi; it comes from the Greek for "hidden sphere". A few species in the Cryptococcus genus cause a disease called cryptococcosis.

The viridans streptococci are a large group of commensal streptococcal Gram-positive bacteria species that are α-hemolytic, producing a green coloration on blood agar plates. The pseudo-taxonomic term "Streptococcus viridans" is often used to refer to this group of species, but writers who do not like to use the pseudotaxonomic term prefer the terms viridans streptococci, viridans group streptococci (VGS), or viridans streptococcal species.

Moraxella catarrhalis is a fastidious, nonmotile, Gram-negative, aerobic, oxidase-positive diplococcus that can cause infections of the respiratory system, middle ear, eye, central nervous system, and joints of humans. It causes the infection of the host cell by sticking to the host cell using trimeric autotransporter adhesins.

Staphylococcus epidermidis is a Gram-positive bacterium, and one of over 40 species belonging to the genus Staphylococcus. It is part of the normal human flora, typically the skin flora, and less commonly the mucosal flora and also found in marine sponges. It is a facultative anaerobic bacteria. Although S. epidermidis is not usually pathogenic, patients with compromised immune systems are at risk of developing infection. These infections are generally hospital-acquired. S. epidermidis is a particular concern for people with catheters or other surgical implants because it is known to form biofilms that grow on these devices. Being part of the normal skin flora, S. epidermidis is a frequent contaminant of specimens sent to the diagnostic laboratory.

A diplococcus is a round bacterium that typically occurs in the form of two joined cells.

Burkholderia pseudomallei is a Gram-negative, bipolar, aerobic, motile rod-shaped bacterium. It is a soil-dwelling bacterium endemic in tropical and subtropical regions worldwide, particularly in Thailand and northern Australia. It infects humans and other animals and causes the disease melioidosis. It is also capable of infecting plants.
Elizabethkingia meningoseptica is a Gram-negative, rod-shaped bacterium widely distributed in nature. It may be normally present in fish and frogs; it may be isolated from chronic infectious states, as in the sputum of cystic fibrosis patients. In 1959, American bacteriologist Elizabeth O. King was studying unclassified bacteria associated with pediatric meningitis at the Centers for Disease Control and Prevention in Atlanta, when she isolated an organism that she named Flavobacterium meningosepticum. In 1994, it was reclassified in the genus Chryseobacterium and renamed Chryseobacterium meningosepticum(chryseos = "golden" in Greek, so Chryseobacterium means a golden/yellow rod similar to Flavobacterium). In 2005, a 16S rRNA phylogenetic tree of Chryseobacteria showed that C. meningosepticum along with C. miricola were close to each other but outside the tree of the rest of the Chryseobacteria and were then placed in a new genus Elizabethkingia named after the original discoverer of F. meningosepticum.
Capnocytophaga is a genus of Gram-negative bacteria. Normally found in the oropharyngeal tract of mammals, they are involved in the pathogenesis of some animal bite wounds and periodontal diseases.

Thayer–Martin agar is a Mueller–Hinton agar with 5% chocolate sheep blood and antibiotics. It is used for culturing and primarily isolating pathogenic Neisseria bacteria, including Neisseria gonorrhoeae and Neisseria meningitidis, as the medium inhibits the growth of most other microorganisms. When growing Neisseria meningitidis, one usually starts with a normally sterile body fluid, so a plain chocolate agar is used. Thayer–Martin agar was initially developed in 1964, with an improved formulation published in 1966.
Clostridium innocuum is an anaerobic, non-motile, gram-positive bacterium that reproduces by sporulation. While there are over 130 species of Clostridium, C. innocuum is the third most commonly isolated. Although it is not normally considered an aggressive human pathogen, it has been isolated in some disease processes. C. innocuum and other Clostridium line the oropharynx and gastrointestinal tract, and are considered normal gut flora.

Clostridium tertium is an anaerobic, motile, gram-positive bacterium. Although it can be considered an uncommon pathogen in humans, there has been substantial evidence of septic episodes in human beings. C. tertium is easily decolorized in Gram-stained smears and can be mistaken for a Gram-negative organism. However, C.tertium does not grow on selective media for Gram-negative organisms.
Neisseria bacilliformis is a bacterium commonly found living as a commensal in the mucous membranes of mammals. However, depending on host immunocompetence, there have been documented cases of N. bacilliformis infections of the respiratory tract and oral cavity thus making it an opportunistic pathogen. It was originally isolated from patients being treated in a cancer center. Rarely, a more serious infection such as endocarditis can occur often as a result of a predisposing condition.
Staphylococcus schleiferi is a Gram-positive, cocci-shaped bacterium of the family Staphylococcaceae. It is facultatively anaerobic, coagulase-variable, and can be readily cultured on blood agar where the bacterium tends to form opaque, non-pigmented colonies and beta (β) hemolysis. There exists two subspecies under the species S. schleiferi: Staphylococcus schleiferi subsp. schleiferi and Staphylococcus schleiferi subsp. coagulans.

The N.Y.C medium or GC medium agar is used for isolating Gonococci.

Granada medium is a selective and differential culture medium designed to selectively isolate Streptococcus agalactiae and differentiate it from other microorganisms. Granada Medium was developed by Dr. Manuel Rosa-Fraile et al. at the Service of Microbiology in the Hospital Virgen de las Nieves in Granada (Spain).
Diagnostic microbiology is the study of microbial identification. Since the discovery of the germ theory of disease, scientists have been finding ways to harvest specific organisms. Using methods such as differential media or genome sequencing, physicians and scientists can observe novel functions in organisms for more effective and accurate diagnosis of organisms. Methods used in diagnostic microbiology are often used to take advantage of a particular difference in organisms and attain information about what species it can be identified as, which is often through a reference of previous studies. New studies provide information that others can reference so that scientists can attain a basic understanding of the organism they are examining.