A melanocytic nevus is usually a noncancerous condition of pigment-producing skin cells. It is a type of melanocytic tumor that contains nevus cells. Some sources equate the term mole with "melanocytic nevus", but there are also sources that equate the term mole with any nevus form.

A birthmark is a congenital, benign irregularity on the skin which is present at birth or appears shortly after birth—usually in the first month. Birthmarks can occur anywhere on the skin. They are caused by overgrowth of blood vessels, melanocytes, smooth muscle, fat, fibroblasts, or keratinocytes.

A Mongolian spot, also known as slate grey nevus or congenital dermal melanocytosis, is a benign, flat, congenital birthmark with wavy borders and an irregular shape. In 1883, it was described and named after Mongolians by Erwin Bälz, a German anthropologist based in Japan, who erroneously believed it to be most prevalent among his Mongolian patients. It normally disappears three to five years after birth and almost always by puberty. The most common color is blue, although they can be blue-gray, blue-black or deep brown.

Nevus is a nonspecific medical term for a visible, circumscribed, chronic lesion of the skin or mucosa. The term originates from nævus, which is Latin for "birthmark"; however, a nevus can be either congenital or acquired. Common terms, including mole, birthmark, and beauty mark, are used to describe nevi, but these terms do not distinguish specific types of nevi from one another.

Melasma is a tan or dark skin discoloration. Melasma is thought to be caused by sun exposure, genetic predisposition, hormone changes, and skin irritation. Although it can affect anyone, it is particularly common in women, especially pregnant women and those who are taking oral or patch contraceptives or hormone replacement therapy medications.

Lentigo maligna is where melanocyte cells have become malignant and grow continuously along the stratum basale of the skin, but have not invaded below the epidermis. Lentigo maligna is not the same as lentigo maligna melanoma, as detailed below. It typically progresses very slowly and can remain in a non-invasive form for years.

The congenital melanocytic nevus is a type of melanocytic nevus found in infants at birth. This type of birthmark occurs in an estimated 1% of infants worldwide; it is located in the area of the head and neck 15% of the time.

Becker's nevus is a benign skin disorder predominantly affecting males. The nevus can be present at birth, but more often shows up around puberty. It generally first appears as an irregular pigmentation on the torso or upper arm, and gradually enlarges irregularly, becoming thickened and often hairy (hypertrichosis). The nevus is due to an overgrowth of the epidermis, pigment cells (melanocytes), and hair follicles. This form of nevus was first documented in 1948 by American dermatologist Samuel William Becker (1894–1964).

Tattoo removal is the process of removing an unwanted tattoo. The process of tattooing generally creates permanent markings in the skin, but people have attempted many methods to try to hide or destroy tattoos.

A blue nevus is a type of coloured mole, typically a single well-defined blue-black bump.

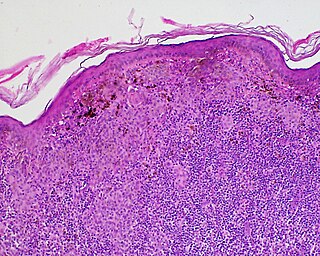
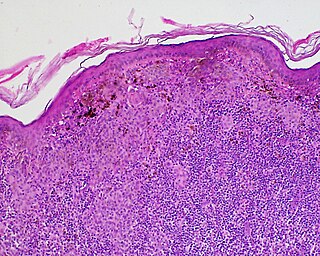
Skin biopsy is a biopsy technique in which a skin lesion is removed to be sent to a pathologist to render a microscopic diagnosis. It is usually done under local anesthetic in a physician's office, and results are often available in 4 to 10 days. It is commonly performed by dermatologists. Skin biopsies are also done by family physicians, internists, surgeons, and other specialties. However, performed incorrectly, and without appropriate clinical information, a pathologist's interpretation of a skin biopsy can be severely limited, and therefore doctors and patients may forgo traditional biopsy techniques and instead choose Mohs surgery.
Roy G. Geronemus is an American dermatologist in the field of laser treatment of skin disorders.
Halo nevus is a mole that is surrounded by a depigmented ring or 'halo'.

A benign melanocytic nevus is a cutaneous condition characterised by well-circumscribed, pigmented, round or ovoid lesions, generally measuring from 2 to 6 mm in diameter. A benign melanocytic nevus may feature hair or pigmentation as well.
Pseudomelanoma is a cutaneous condition in which melanotic skin lesions clinically resemble a superficial spreading melanoma at the site of a recent shave removal of a melanocytic nevus.
Postinflammatory hypopigmentation is a cutaneous condition characterized by decreased pigment in the skin following inflammation of the skin.
Oral pigmentation is asymptomatic and does not usually cause any alteration to the texture or thickness of the affected area. The colour can be uniform or speckled and can appear solitary or as multiple lesions. Depending on the site, depth, and quantity of pigment, the appearance can vary considerably.

Nevus depigmentosus is a loss of pigment in the skin which can be easily differentiated from vitiligo. Although age factor has not much involvement in the nevus depigmentosus but in about 19% of the cases these are noted at birth. Their size may however grow in proportion to growth of the body. The distribution is also fairly stable and are nonprogressive hypopigmented patches. The exact cause of nevus depigmentosus is still not clearly understood. A sporadic defect in the embryonic development has been suggested to be a causative factor. It has been described as "localised albinism", though this is incorrect.

Supernumerary nipples–uropathies–Becker's nevus syndrome is a skin condition that may be associated with genitourinary tract abnormalities. Supernumerary nipples, also referred to as polythelia or accessory nipples, is a pigmented lesion of the skin that is present at birth. This pigmentation usually occurs along the milk lines, which are the precursors to breast and nipple development. Clinically, this congenital condition is generally considered benign, but some studies have suggested there may be an association with kidney diseases and cancers of the urogenital system.
Mucinous nevus is a rare cutaneous condition characterized by hamartoma that can be congenital or acquired. Mucinous nevus presents as multiple skin-coloured or brown asymptomatic papules or plaques. Mucinous nevus is diagnosed based of histological features. Treatment is not needed.