Related Research Articles

Bornholm disease, also known as epidemic pleurodynia, is a condition characterized by myositis of the abdomen or chest caused by the Coxsackie B virus or other viruses. The myositis manifests as an intermittent stabbing pain in the musculature that is seen primarily in children and young adults.
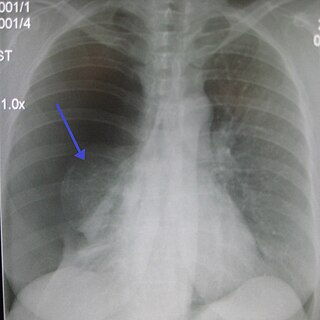
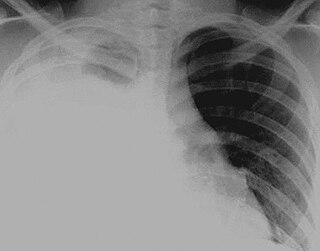
A pneumothorax is an abnormal collection of air in the pleural space between the lung and the chest wall. Symptoms typically include sudden onset of sharp, one-sided chest pain and shortness of breath. In a minority of cases, a one-way valve is formed by an area of damaged tissue, and the amount of air in the space between chest wall and lungs increases; this is called a tension pneumothorax. This can cause a steadily worsening oxygen shortage and low blood pressure. This leads to a type of shock called obstructive shock, which can be fatal unless reversed. Very rarely, both lungs may be affected by a pneumothorax. It is often called a "collapsed lung", although that term may also refer to atelectasis.

Pleurisy, also known as pleuritis, is inflammation of the membranes that surround the lungs and line the chest cavity (pleurae). This can result in a sharp chest pain while breathing. Occasionally the pain may be a constant dull ache. Other symptoms may include shortness of breath, cough, fever or weight loss, depending on the underlying cause.

A pleural effusion is accumulation of excessive fluid in the pleural space, the potential space that surrounds each lung. Under normal conditions, pleural fluid is secreted by the parietal pleural capillaries at a rate of 0.01 millilitre per kilogram weight per hour, and is cleared by lymphatic absorption leaving behind only 5–15 millilitres of fluid, which helps to maintain a functional vacuum between the parietal and visceral pleurae. Excess fluid within the pleural space can impair inspiration by upsetting the functional vacuum and hydrostatically increasing the resistance against lung expansion, resulting in a fully or partially collapsed lung.

Pleural empyema is a collection of pus in the pleural cavity caused by microorganisms, usually bacteria. Often it happens in the context of a pneumonia, injury, or chest surgery. It is one of the various kinds of pleural effusion. There are three stages: exudative, when there is an increase in pleural fluid with or without the presence of pus; fibrinopurulent, when fibrous septa form localized pus pockets; and the final organizing stage, when there is scarring of the pleura membranes with possible inability of the lung to expand. Simple pleural effusions occur in up to 40% of bacterial pneumonias. They are usually small and resolve with appropriate antibiotic therapy. If however an empyema develops additional intervention is required.

A chest tube is a surgical drain that is inserted through the chest wall and into the pleural space or the mediastinum in order to remove clinically undesired substances such as air (pneumothorax), excess fluid, blood (hemothorax), chyle (chylothorax) or pus (empyema) from the intrathoracic space. An intrapleural chest tube is also known as a Bülau drain or an intercostal catheter (ICC), and can either be a thin, flexible silicone tube, or a larger, semi-rigid, fenestrated plastic tube, which often involves a flutter valve or underwater seal.

A chest radiograph, called a chest X-ray (CXR), or chest film, is a projection radiograph of the chest used to diagnose conditions affecting the chest, its contents, and nearby structures. Chest radiographs are the most common film taken in medicine.

A hemothorax is an accumulation of blood within the pleural cavity. The symptoms of a hemothorax may include chest pain and difficulty breathing, while the clinical signs may include reduced breath sounds on the affected side and a rapid heart rate. Hemothoraces are usually caused by an injury, but they may occur spontaneously due to cancer invading the pleural cavity, as a result of a blood clotting disorder, as an unusual manifestation of endometriosis, in response to a collapsed lung, or rarely in association with other conditions.
Hydrothorax is a type of pleural effusion in which transudate accumulates in the pleural cavity. This condition is most likely to develop secondary to congestive heart failure, following an increase in hydrostatic pressure within the lungs. More rarely, hydrothorax can develop in 10% of patients with ascites which is called hepatic hydrothorax. It is often difficult to manage in end-stage liver failure and often fails to respond to therapy.
A pericardial friction rub, also pericardial rub, is an audible medical sign used in the diagnosis of pericarditis. Upon auscultation, this sign is an extra heart sound of to-and-fro character, typically with three components, two systolic and one diastolic. It resembles the sound of squeaky leather and often is described as grating, scratching, or rasping. The sound seems very close to the ear and may seem louder than or may even mask the other heart sounds. The sound usually is best heard between the apex and sternum but may be widespread.
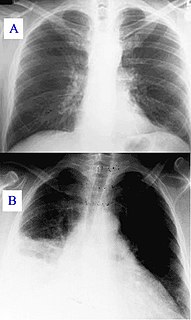
A pulmonary consolidation is a region of normally compressible lung tissue that has filled with liquid instead of air. The condition is marked by induration of a normally aerated lung. It is considered a radiologic sign. Consolidation occurs through accumulation of inflammatory cellular exudate in the alveoli and adjoining ducts. The liquid can be pulmonary edema, inflammatory exudate, pus, inhaled water, or blood. Consolidation must be present to diagnose pneumonia: the signs of lobar pneumonia are characteristic and clinically referred to as consolidation.
Egophony is an increased resonance of voice sounds heard when auscultating the lungs, often caused by lung consolidation and fibrosis. It is due to enhanced transmission of high-frequency sound across fluid, such as in abnormal lung tissue, with lower frequencies filtered out. It results in a high-pitched nasal or bleating quality in the affected person's voice.
Fremitus is a vibration transmitted through the body. In common medical usage, it usually refers to assessment of the lungs by either the vibration intensity felt on the chest wall and/or heard by a stethoscope on the chest wall with certain spoken words, although there are several other types.
Rheumatoid pleuritis, a form of pleural effusion, is an uncommon complication of rheumatoid arthritis, occurring in 2-3% of patients Rheumatoid pleura most often appears as an erythematous exanthema, discoloration, or gray discoloration and may grow into a tender, inflamed mass.

Acute pericarditis is a type of pericarditis usually lasting less than 6 weeks. It is the most common condition affecting the pericardium.
Pleural disease occurs in the pleural space, which is the thin fluid-filled area in between the two pulmonary pleurae in the human body. There are several disorders and complications that can occur within the pleural area, and the surrounding tissues in the lung.
Rheumatoid lung disease is a disease of the lung associated with RA, rheumatoid arthritis. Rheumatoid lung disease is characterized by pleural effusion, pulmonary fibrosis, lung nodules and pulmonary hypertension. Common symptoms associated with the disease include shortness of breath, cough, chest pain and fever. It is estimated that about one quarter of people with rheumatoid arthritis develop this disease, which are more likely to develop among elderly men with a history of smoking.

Postpericardiotomy syndrome (PPS) is a medical syndrome referring to an immune phenomenon that occurs days to months after surgical incision of the pericardium. PPS can also be caused after a trauma, a puncture of the cardiac or pleural structures, after percutaneous coronary intervention, or due to pacemaker or pacemaker wire placement.

The pulmonary pleurae are the two opposing layers of serous membrane overlying the lungs and the inside of the surrounding chest walls.

Chest pain in children is the pain felt in the chest by infants, children and adolescents. In most cases the pain is not associated with the heart. It is primarily identified by the observance or report of pain by the infant, child or adolescent by reports of distress by parents or caregivers. Chest pain is not uncommon in children. Many children are seen in ambulatory clinics, emergency departments and hospitals and cardiology clinics. Most often there is a benign cause for the pain for most children. Some have conditions that are serious and possibly life-threatening. Chest pain in pediatric patients requires careful physical examination and a detailed history that would indicate the possibility of a serious cause. Studies of pediatric chest pain are sparse. It has been difficult to create evidence-based guidelines for evaluation.