Mumps is a viral disease caused by the mumps virus. Initial symptoms are non-specific and include fever, headache, malaise, muscle pain, and loss of appetite. These symptoms are usually followed by painful swelling of the parotid glands, called parotitis, which is the most common symptom of infection. Symptoms typically occur 16 to 18 days after exposure to the virus and resolve within two weeks. About one third of infections are asymptomatic.

Scarlet fever is a disease resulting from a group A streptococcus infection, also known as Streptococcus pyogenes. The signs and symptoms include a sore throat, fever, headaches, swollen lymph nodes, and a characteristic rash. The rash is red and feels like sandpaper and the tongue may be red and bumpy. It most commonly affects children between five and 15 years of age.

Staphylococcus aureus is a Gram-positive, round-shaped bacterium, a member of the Firmicutes, and is a usual member of the microbiota of the body, frequently found in the upper respiratory tract and on the skin. It is often positive for catalase and nitrate reduction and is a facultative anaerobe that can grow without the need for oxygen. Although S. aureus usually acts as a commensal of the human microbiota it can also become an opportunistic pathogen, being a common cause of skin infections including abscesses, respiratory infections such as sinusitis, and food poisoning. Pathogenic strains often promote infections by producing virulence factors such as potent protein toxins, and the expression of a cell-surface protein that binds and inactivates antibodies. The emergence of antibiotic-resistant strains of S. aureus such as methicillin-resistant S. aureus (MRSA) is a worldwide problem in clinical medicine. Despite much research and development, no vaccine for S. aureus has been approved.

Hydrocephalus is a condition in which an accumulation of cerebrospinal fluid (CSF) occurs within the brain. This typically causes increased pressure inside the skull. Older people may have headaches, double vision, poor balance, urinary incontinence, personality changes, or mental impairment. In babies, it may be seen as a rapid increase in head size. Other symptoms may include vomiting, sleepiness, seizures, and downward pointing of the eyes.

Nephritis is inflammation of the kidneys and may involve the glomeruli, tubules, or interstitial tissue surrounding the glomeruli and tubules.

Acute bone and joint infections namely acute suppurative arthritis and acute hematogenous osteomyelitis mainly occur in the children and adolescences. Acute suppurative arthritis or septic arthritis or joint infection or infectious arthritis is the invasion of a joint by an infectious agent resulting in joint inflammation. Generally speaking, symptoms typically include redness, heat and pain in a single joint associated with a decreased ability to move the joint. Onset is usually rapid. Other symptoms may include fever, weakness and headache. Occasionally, more than one joint may be involved especially in neonates and younger children. In neonates, infants i.e. during the first year of life and toddlers, the signs and symptoms of septic arthritis can be deceptive and mimic other infectious and non-infectious disorders.

Infective endocarditis is an infection of the inner surface of the heart, usually the valves. Signs and symptoms may include fever, small areas of bleeding into the skin, heart murmur, feeling tired, and low red blood cell count. Complications may include backward blood flow in the heart, heart failure – the heart struggling to pump a sufficient amount of blood to meet the body's needs, abnormal electrical conduction in the heart, stroke, and kidney failure.

Leptospirosis is a blood infection caused by the bacteria Leptospira. Signs and symptoms can range from none to mild to severe. Weil's disease, the acute, severe form of leptospirosis, causes the infected individual to become jaundiced, develop kidney failure, and bleed. Bleeding from the lungs associated with leptospirosis is known as "severe pulmonary haemorrhage syndrome".

IgA nephropathy (IgAN), also known as Berger's disease, or synpharyngitic glomerulonephritis, is a disease of the kidney and the immune system; specifically it is a form of glomerulonephritis or an inflammation of the glomeruli of the kidney. Aggressive Berger's disease can attack other major organs, such as the liver, skin and heart.

Henoch–Schönlein purpura (HSP), also known as IgA vasculitis, is a disease of the skin, mucous membranes, and sometimes other organs that most commonly affects children. In the skin, the disease causes palpable purpura, often with joint pain and abdominal pain. With kidney involvement, there may be a loss of small amounts of blood and protein in the urine, but this usually goes unnoticed; in a small proportion of cases, the kidney involvement proceeds to chronic kidney disease. HSP is often preceded by an infection, such as a throat infection.
Glomerulonephritis (GN) is a term used to refer to several kidney diseases. Many of the diseases are characterised by inflammation either of the glomeruli or of the small blood vessels in the kidneys, hence the name, but not all diseases necessarily have an inflammatory component.

Pyelonephritis is inflammation of the kidney, typically due to a bacterial infection. Symptoms most often include fever and flank tenderness. Other symptoms may include nausea, burning with urination, and frequent urination. Complications may include pus around the kidney, sepsis, or kidney failure.
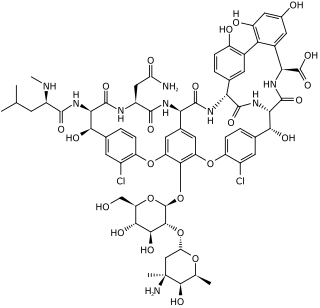
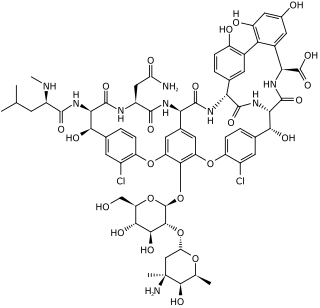
Glycopeptide antibiotics are a class of drugs of microbial origin that are composed of glycosylated cyclic or polycyclic nonribosomal peptides. Significant glycopeptide antibiotics include the anti-infective antibiotics vancomycin, teicoplanin, telavancin, ramoplanin and decaplanin, corbomycin, complestatin and the antitumor antibiotic bleomycin. Vancomycin is used if infection with methicillin-resistant Staphylococcus aureus (MRSA) is suspected.

Lupus nephritis is an inflammation of the kidneys caused by systemic lupus erythematosus (SLE), an autoimmune disease. It is a type of glomerulonephritis in which the glomeruli become inflamed. As the result of SLE, the cause of glomerulonephritis is said to be secondary and has a different pattern and outcome from conditions with a primary cause originating in the kidney.

Staphylococcus epidermidis is a Gram-positive bacterium, and one of over 40 species belonging to the genus Staphylococcus. It is part of the normal human flora, typically the skin flora, and less commonly the mucosal flora. It is a facultative anaerobic bacteria. Although S. epidermidis is not usually pathogenic, patients with compromised immune systems are at risk of developing infection. These infections are generally hospital-acquired. S. epidermidis is a particular concern for people with catheters or other surgical implants because it is known to form biofilms that grow on these devices. Being part of the normal skin flora, S. epidermidis is a frequent contaminant of specimens sent to the diagnostic laboratory.
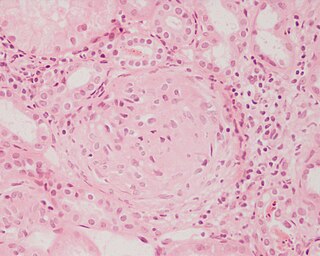
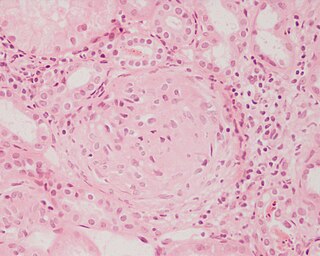
Interstitial nephritis, also known as tubulointerstitial nephritis, is inflammation of the area of the kidney known as the renal interstitium, which consists of a collection of cells, extracellular matrix, and fluid surrounding the renal tubules. In addition to providing a scaffolding support for the tubular architecture, the interstitium has been shown to participate in the fluid and electrolyte exchange as well as endocrine functions of the kidney.

Acute proliferative glomerulonephritis is a disorder of the small blood vessels of the kidney. It is a common complication of bacterial infections, typically skin infection by Streptococcus bacteria types 12, 4 and 1 (impetigo) but also after streptococcal pharyngitis, for which it is also known as postinfectious glomerulonephritis (PIGN) or poststreptococcal glomerulonephritis (PSGN). It can be a risk factor for future albuminuria. In adults, the signs and symptoms of infection may still be present at the time when the kidney problems develop, and the terms infection-related glomerulonephritis or bacterial infection-related glomerulonephritis are also used. Acute glomerulonephritis resulted in 19,000 deaths in 2013, down from 24,000 deaths in 1990 worldwide.

Cerebral shunts are commonly used to treat hydrocephalus, the swelling of the brain due to excess buildup of cerebrospinal fluid (CSF). If left unchecked, the cerebrospinal fluid can build up leading to an increase in intracranial pressure (ICP) which can lead to intracranial hematoma, cerebral edema, crushed brain tissue or herniation. The cerebral shunt can be used to alleviate or prevent these problems in patients who suffer from hydrocephalus or other related diseases.

Lupus, technically known as systemic lupus erythematosus (SLE), is an autoimmune disease in which the body's immune system mistakenly attacks healthy tissue in many parts of the body. Symptoms vary between people and may be mild to severe. Common symptoms include painful and swollen joints, fever, chest pain, hair loss, mouth ulcers, swollen lymph nodes, feeling tired, and a red rash which is most commonly on the face. Often there are periods of illness, called flares, and periods of remission during which there are few symptoms.
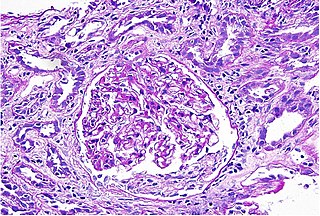
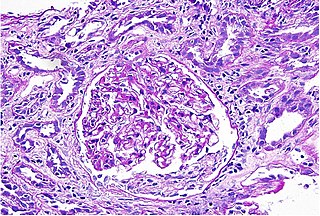
Diffuse proliferative glomerulonephritis (DPGN) is a type of glomerulonephritis that is the most serious form of renal lesions in SLE and is also the most common, occurring in 35% to 60% of patients. Most of the glomeruli show endothelial and mesangial proliferation, affecting the entire glomerulus, leading to diffuse hypercellularity of the glomeruli, producing in some cases epithelial crescents that fill Bowman's space. When extensive, immune complexes create an overall thickening of the capillary wall, resembling rigid "wire loops" on routine light microscopy. Electron microscopy reveals electron-dense subendothelial immune complexes. Immune complexes can be visualized by staining with fluorescent antibodies directed against immunoglobulins or complement, resulting in a granular fluorescent staining pattern. In due course, glomerular injury gives rise to scarring (glomerulosclerosis). Most of these patients have hematuria with moderate to severe proteinuria, hypertension, and renal insufficiency.