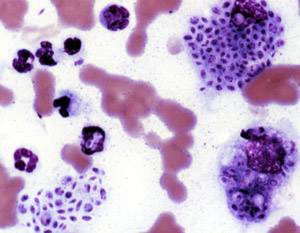
Candidiasis is a fungal infection due to any species of the genus Candida. When it affects the mouth, in some countries it is commonly called thrush. Signs and symptoms include white patches on the tongue or other areas of the mouth and throat. Other symptoms may include soreness and problems swallowing. When it affects the vagina, it may be referred to as a yeast infection or thrush. Signs and symptoms include genital itching, burning, and sometimes a white "cottage cheese-like" discharge from the vagina. Yeast infections of the penis are less common and typically present with an itchy rash. Very rarely, yeast infections may become invasive, spreading to other parts of the body. This may result in fevers, among other symptoms, depending on the parts involved.

An antifungal medication, also known as an antimycotic medication, is a pharmaceutical fungicide or fungistatic used to treat and prevent mycosis such as athlete's foot, ringworm, candidiasis (thrush), serious systemic infections such as cryptococcal meningitis, and others. Such drugs are usually obtained by a doctor's prescription, but a few are available over the counter (OTC). The evolution of antifungal resistance is a growing threat to health globally.
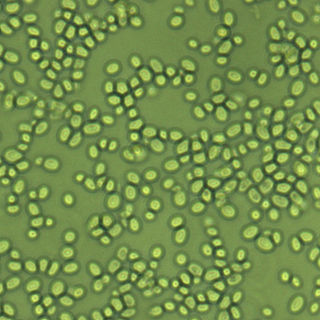
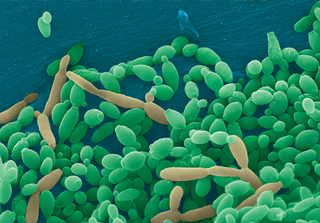
Candida is a genus of yeasts. It is the most common cause of fungal infections worldwide and the largest genus of medically important yeast.

Coccidioides immitis is a pathogenic fungus that resides in the soil in certain parts of the southwestern United States, northern Mexico, and a few other areas in the Western Hemisphere.
Sporotrichosis, also known as rose handler's disease, is a fungal infection that may be localised to skin, lungs, bone and joint, or become systemic. It presents with firm painless nodules that later ulcerate. Following initial exposure to Sporothrix schenckii, the disease typically progresses over a period of a week to several months. Serious complications may develop in people who have a weakened immune system.
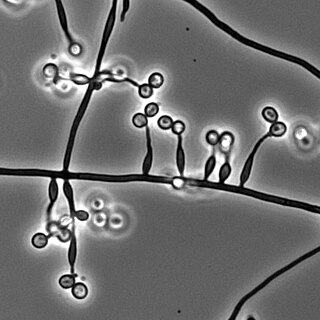
Pichia kudriavzevii is a budding yeast involved in chocolate production. P. kudriavzevii is an emerging fungal nosocomial pathogen primarily found in the immunocompromised and those with hematological malignancies. It has natural resistance to fluconazole, a standard antifungal agent. It is most often found in patients who have had prior fluconazole exposure, sparking debate and conflicting evidence as to whether fluconazole should be used prophylactically. Mortality due to P. kudriavzevii fungemia is much higher than the more common C. albicans. Other Candida species that also fit this profile are C. parapsilosis, C. glabrata, C. tropicalis, C. guillermondii and C. rugosa.
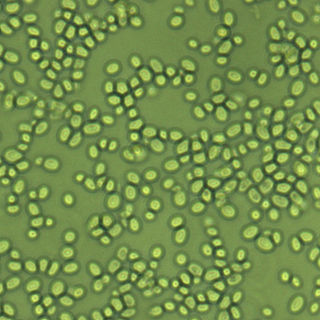
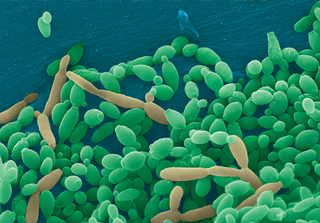
Nakaseomyces glabratus is a species of haploid yeast of the genus Nakaseomyces, previously known as Candida glabrata. Despite the fact that no sexual life cycle has been documented for this species, N. glabratus strains of both mating types are commonly found. C. glabrata is generally a commensal of human mucosal tissues, but in today's era of wider human immunodeficiency from various causes, N. glabratus is often the second or third most common cause of candidiasis as an opportunistic pathogen. Infections caused by N. glabratus can affect the urogenital tract or even cause systemic infections by entrance of the fungal cells in the bloodstream (Candidemia), especially prevalent in immunocompromised patients.
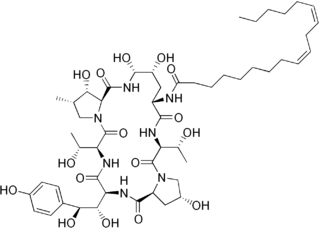
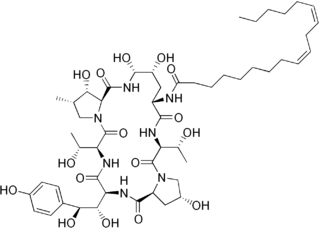
Echinocandins are a class of antifungal drugs that inhibit the synthesis of β-glucan in the fungal cell wall via noncompetitive inhibition of the enzyme 1,3-β glucan synthase. The class has been termed the "penicillin of antifungals," along with the related papulacandins, as their mechanism of action resembles that of penicillin in bacteria. β-glucans are carbohydrate polymers that are cross-linked with other fungal cell wall components, the fungal equivalent to bacterial peptidoglycan. Caspofungin, micafungin, and anidulafungin are semisynthetic echinocandin derivatives with limited clinical use due to their solubility, antifungal spectrum, and pharmacokinetic properties.

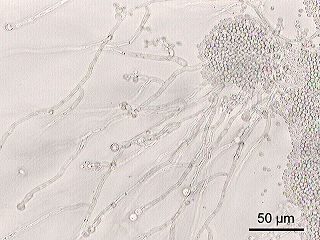
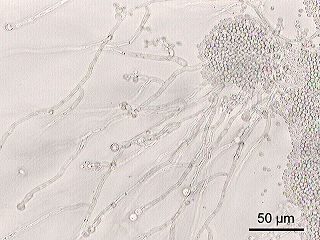
Geotrichum is a genus of fungi found worldwide in soil, water, air, and sewage, as well as in plants, cereals, and dairy products; it is also commonly found in normal human flora and is isolated from sputum and feces. It was first described in 1809 by Johann Heinrich Friedrich Link.
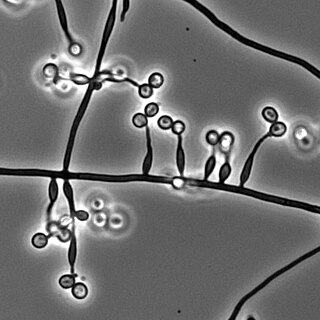
Exophiala jeanselmei is a saprotrophic fungus in the family Herpotrichiellaceae. Four varieties have been discovered: Exophiala jeanselmei var. heteromorpha, E. jeanselmei var. lecanii-corni, E. jeanselmei var. jeanselmei, and E. jeanselmei var. castellanii. Other species in the genus Exophiala such as E. dermatitidis and E. spinifera have been reported to have similar annellidic conidiogenesis and may therefore be difficult to differentiate.

Trichosporon is a genus of anamorphic fungi in the family Trichosporonaceae. All species of Trichosporon are yeasts with no known teleomorphs. Most are typically isolated from soil, but several species occur as a natural part of the skin microbiota of humans and other animals. Proliferation of Trichosporon yeasts in the hair can lead to an unpleasant but non-serious condition known as white piedra. Trichosporon species can also cause severe opportunistic infections (trichosporonosis) in immunocompromised individuals.

Exophiala dermatitidis is a thermophilic black yeast, and a member of the Herpotrichiellaceae. While the species is only found at low abundance in nature, metabolically active strains are commonly isolated in saunas, steam baths, and dish washers. Exophiala dermatitidis only rarely causes infection in humans, however cases have been reported around the world. In East Asia, the species has caused lethal brain infections in young and otherwise healthy individuals. The fungus has been known to cause cutaneous and subcutaneous phaeohyphomycosis, and as a lung colonist in people with cystic fibrosis in Europe. In 2002, an outbreak of systemic E. dermatitidis infection occurred in women who had received contaminated steroid injections at North Carolina hospitals.
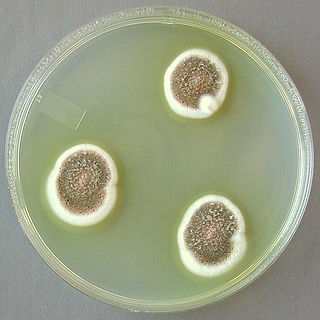
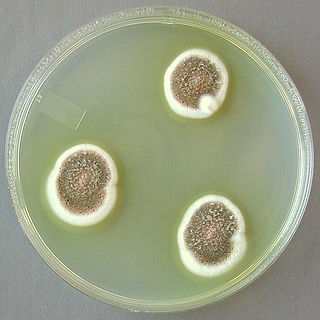
Aspergillus ustus is a microfungus and member of the division Ascomycota. It is commonly found in indoor environments and soil. Isolated cases of human infection resulting from A. ustus have been described; however the majority of these are nail infections.
Scedosporiosis is the general name for any mycosis – i.e., fungal infection – caused by a fungus from the genus Scedosporium. Current population-based studies suggest Scedosporium prolificans and Scedosporium apiospermum to be among the most common infecting agents from the genus, although infections caused by other members thereof are not unheard of. The latter is an asexual form (anamorph) of another fungus, Pseudallescheria boydii. The former is a "black yeast", currently not characterized as well, although both of them have been described as saprophytes.
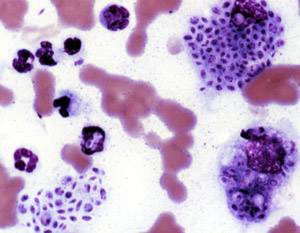
Histoplasma duboisii is a saprotrophic fungus responsible for the invasive infection known as African histoplasmosis. This species is a close relative of Histoplasma capsulatum, the agent of classical histoplasmosis, and the two occur in similar habitats. Histoplasma duboisii is restricted to continental Africa and Madagascar, although scattered reports have arisen from other places usually in individuals with an African travel history. Like, H. capsulatum, H. duboisii is dimorphic – growing as a filamentous fungus at ambient temperature and a yeast at body temperature. It differs morphologically from H. capsulatum by the typical production of a large-celled yeast form. Both agents cause similar forms of disease, although H. duboisii predominantly causes cutaneous and subcutaneous disease in humans and non-human primates. The agent responds to many antifungal drug therapies used to treat serious fungal diseases.

Candida auris is a species of fungus that grows as yeast. It is one of the few species of the genus Candida which cause candidiasis in humans. Often, candidiasis is acquired in hospitals by patients with weakened immune systems. C. auris can cause invasive candidiasis (fungemia) in which the bloodstream, the central nervous system, and internal organs are infected. It has attracted widespread attention because of its multiple drug resistance. Treatment is also complicated because it is easily misidentified as other Candida species.
Invasive candidiasis is an infection (candidiasis) that can be caused by various species of Candida yeast. Unlike Candida infections of the mouth and throat or vagina, invasive candidiasis is a serious, progressive, and potentially fatal infection that can affect the blood (fungemia), heart, brain, eyes, bones, and other parts of the body.
Candida tropicalis is a species of yeast in the genus Candida. It is a common pathogen in neutropenic hosts, in whom it may spread through the bloodstream to peripheral organs. For invasive disease, treatments include amphotericin B, echinocandins, or extended-spectrum triazole antifungals.
Metarhizium granulomatis is a fungus in the family Clavicipitaceae associated with systemic mycosis in veiled chameleons. The genus Metarhizium is known to infect arthropods, and collectively are referred to green-spored asexual pathogenic fungi. This species grows near the roots of plants and has been reported as an agent of disease in captive veiled chameleons. The etymology of the species epithet, "granulomatis" refers to the ability of the fungus to cause granulomatous disease in susceptible reptiles.
Candida haemulonii is a yeast fungal pathogen that is known to cause infections in humans. C. haemulonii is an emerging opportunistic pathogen that is found in hospitals and healthcare settings. Infections are difficult to treat because the fungus has resistance to antifungal agents. Since its emergence, little research has been conducted on this fungus. However, in recent years, research has been conducted to help identify the various properties of C. haemulonii.