Jules Jean Baptiste Vincent Bordet was a Belgian immunologist and microbiologist. The bacterial genus Bordetella is named after him. The Nobel Prize in Physiology or Medicine was awarded to him in 1919 for his discoveries relating to immunity.
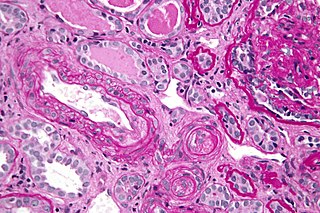
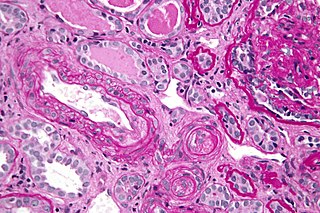
Antiphospholipid syndrome, or antiphospholipid antibody syndrome, is an autoimmune, hypercoagulable state caused by antiphospholipid antibodies. APS can lead to blood clots (thrombosis) in both arteries and veins, pregnancy-related complications, and other symptoms like low platelets, kidney disease, heart disease, and rash. Although the exact etiology of APS is still not clear, genetics is believed to play a key role in the development of the disease. Diagnosis is made based on symptoms and testing, but sometimes research criteria are used to aid in diagnosis. The research criteria for definite APS requires one clinical event and two positive blood test results spaced at least three months apart that detect lupus anticoagulant, anti-apolipoprotein antibodies, and/or anti-cardiolipin antibodies.

HIV tests are used to detect the presence of the human immunodeficiency virus (HIV), the virus that causes acquired immunodeficiency syndrome (AIDS), in serum, saliva, or urine. Such tests may detect antibodies, antigens, or RNA.

August Paul von Wassermann was a German bacteriologist and hygienist.
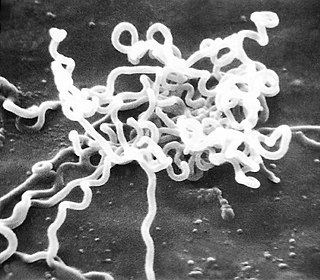
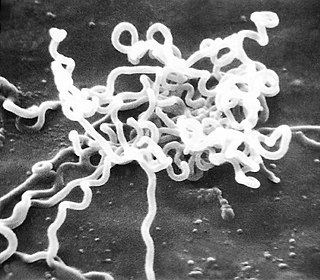
The rapid plasma reagin test is a type of rapid diagnostic test that looks for non-specific antibodies in the blood of the patient that may indicate an infection by syphilis or related non-venereal treponematoses. It is one of several nontreponemal tests for syphilis. The term reagin means that this test does not look for antibodies against the bacterium itself, Treponema pallidum, but rather for antibodies against substances released by cells when they are damaged by T. pallidum. Traditionally, syphilis serologic testing has been performed using a nontreponemal test (NTT) such as the RPR or VDRL test, with positive results then confirmed using a specific treponemal test (TT) such as TPPA or FTA-ABS. This algorithm is currently endorsed by the U.S. Centers for Disease Control and Prevention (CDC). In addition to screening for syphilis, a titer can be used to track the progress of the disease over time and its response to therapy. The traditional algorithm using an NTT followed by a TT remains the standard in many parts of the world.

The Venereal Disease Research Laboratory test (VDRL) is a blood test for syphilis and related non-venereal treponematoses that was developed by the eponymous US laboratory. The VDRL test is used to screen for syphilis, whereas other, more specific tests are used to diagnose the disease.
Serology is the scientific study of serum and other body fluids. In practice, the term usually refers to the diagnostic identification of antibodies in the serum. Such antibodies are typically formed in response to an infection, against other foreign proteins, or to one's own proteins. In either case, the procedure is simple.

Hemolytic disease of the newborn, also known as hemolytic disease of the fetus and newborn, HDN, HDFN, or erythroblastosis fetalis, is an alloimmune condition that develops in a fetus at or around birth, when the IgG molecules produced by the mother pass through the placenta. Among these antibodies are some which attack antigens on the red blood cells in the fetal circulation, breaking down and destroying the cells. The fetus can develop reticulocytosis and anemia. The intensity of this fetal disease ranges from mild to very severe, and fetal death from heart failure can occur. When the disease is moderate or severe, many erythroblasts are present in the fetal blood, earning these forms of the disease the name erythroblastosis fetalis.
The direct and indirect Coombs tests, also known as antiglobulin test (AGT), are blood tests used in immunohematology. The direct Coombs test detects antibodies that are stuck to the surface of the red blood cells. Since these antibodies sometimes destroy red blood cells they can cause anemia; this test can help clarify the condition. The indirect Coombs test detects antibodies that are floating freely in the blood. These antibodies could act against certain red blood cells; the test can be carried out to diagnose reactions to a blood transfusion.
Pinta is a human skin disease caused by infection with the spirochete Treponema carateum, which is morphologically and serologically indistinguishable from the bacterium that causes syphilis. The disease is endemic to Mexico, Central America, and South America.
Octave Gengou was a Belgian bacteriologist. He researched with Jules Bordet the Bordetella pertussis bacteria.

Neurosyphilis is the infection of the central nervous system in a patient with syphilis. In the era of modern antibiotics, the majority of neurosyphilis cases have been reported in HIV-infected patients. Meningitis is the most common neurological presentation in early syphilis. Tertiary syphilis symptoms are exclusively neurosyphilis, though neurosyphilis may occur at any stage of infection.
Autoimmune hemolytic anemia (AIHA) occurs when antibodies directed against the person's own red blood cells (RBCs) cause them to burst (lyse), leading to an insufficient number of oxygen-carrying red blood cells in the circulation. The lifetime of the RBCs is reduced from the normal 100–120 days to just a few days in serious cases. The intracellular components of the RBCs are released into the circulating blood and into tissues, leading to some of the characteristic symptoms of this condition. The antibodies are usually directed against high-incidence antigens, therefore they also commonly act on allogenic RBCs. AIHA is a relatively rare condition, with an incidence of 5–10 cases per 1 million persons per year in the warm-antibody type and 0.45 to 1.9 cases per 1 million persons per year in the cold antibody type. Autoimmune hemolysis might be a precursor of later onset systemic lupus erythematosus.
Paroxysmal cold hemoglobinuria (PCH) or Donath–Landsteiner hemolytic anemia (DLHA) is an autoimmune hemolytic anemia featured by complement-mediated intravascular hemolysis after cold exposure. It can present as an acute non-recurrent postinfectious event in children, or chronic relapsing episodes in adults with hematological malignancies or tertiary syphilis. Described by Julius Donath (1870–1950) and Karl Landsteiner (1868–1943) in 1904, PCH is one of the first clinical entities recognized as an autoimmune disorder.
The complement fixation test is an immunological medical test that can be used to detect the presence of either specific antibody or specific antigen in a patient's serum, based on whether complement fixation occurs. It was widely used to diagnose infections, particularly with microbes that are not easily detected by culture methods, and in rheumatic diseases. However, in clinical diagnostics labs it has been largely superseded by other serological methods such as ELISA and by DNA-based methods of pathogen detection, particularly PCR.
The fluorescent treponemal antibody absorption (FTA-ABS) test is a diagnostic test for syphilis. Using antibodies specific for the Treponema pallidum species, such tests would be assumed to be more specific than non-treponemal testing such as VDRL but have been shown repeatedly to be sensitive but not specific for the diagnosis of neurosyphilis in cerebrospinal fluid (CSF). In addition, FTA-ABS turns positive earlier and remains positive longer than VDRL. Other treponemes, such as T. pertenue, may also produce a positive FTA-ABS. The ABS suffix refers particularly to a processing step used to remove nonspecific antispirochetal antibodies present in normal serum.
A nontreponemal test (NTT) is a blood test for diagnosis of infection with syphilis. Nontreponemal tests are an indirect method in that they detect biomarkers that are released during cellular damage that occurs from the syphilis spirochete. In contrast, treponemal tests look for antibodies that are a direct result of the infection thus, anti-treponeme IgG, IgM and to a lesser degree IgA. Nontreponemal tests are screening tests, very rapid and relatively simple, but need to be confirmed by treponemal tests. Centers for Disease Control and Prevention (CDC)-approved standard tests include the VDRL test, the rapid plasma reagin (RPR) test, the unheated serum reagin (USR) test, and the toluidine red unheated serum test (TRUST). These have mostly replaced the first nontreponemal test, the Wassermann test.

The Treponema pallidum particle agglutination assay is an indirect agglutination assay used for detection and titration of antibodies against the causative agent of syphilis, Treponema pallidum subspecies pallidum. It also detects other treponematoses.

Henry Roy Dean, MD, LL.D, D.Sc, FRCP, also known as Prof. H. R. Dean, was a professor of Pathology at the University of Cambridge and Master of Trinity Hall, Cambridge.

Meningeal syphilis is a chronic form of syphilis infection that affects the central nervous system. Treponema pallidum, a spirochate bacterium, is the main cause of syphilis, which spreads drastically throughout the body and can infect all its systems if not treated appropriately. Treponema pallidum is the main cause of the onset of meningeal syphilis and other treponemal diseases, and it consists of a cytoplasmic and outer membrane that can cause a diverse array of diseases in the central nervous system and brain.