The esophagus or oesophagus, colloquially known also as the food pipe, food tube, or gullet, is an organ in vertebrates through which food passes, aided by peristaltic contractions, from the pharynx to the stomach. The esophagus is a fibromuscular tube, about 25 cm (10 in) long in adults, that travels behind the trachea and heart, passes through the diaphragm, and empties into the uppermost region of the stomach. During swallowing, the epiglottis tilts backwards to prevent food from going down the larynx and lungs. The word oesophagus is from Ancient Greek οἰσοφάγος (oisophágos), from οἴσω (oísō), future form of φέρω + ἔφαγον.

Upper gastrointestinal bleeding is gastrointestinal bleeding (hemorrhage) in the upper gastrointestinal tract, commonly defined as bleeding arising from the esophagus, stomach, or duodenum. Blood may be observed in vomit or in altered form as black stool. Depending on the amount of the blood loss, symptoms may include shock.
Hematemesis is the vomiting of blood. It can be confused with hemoptysis or epistaxis (nosebleed), which are more common. The source is generally the upper gastrointestinal tract, typically above the suspensory muscle of duodenum. It may be caused by ulcers, tumors of the stomach or esophagus, varices, prolonged and vigorous retching, gastroenteritis, ingested blood, or certain drugs.
Coffee ground vomitus refers to a particular appearance of vomit. Within organic heme molecules of red blood cells is the element iron, which oxidizes following exposure to gastric acid. This reaction causes the vomitus to look like ground coffee.
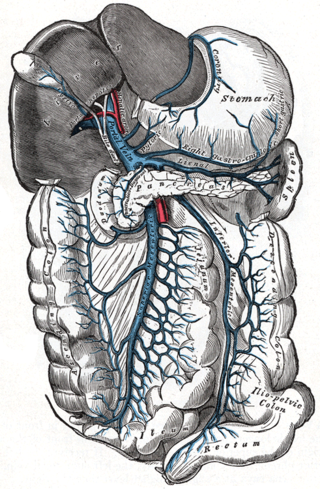
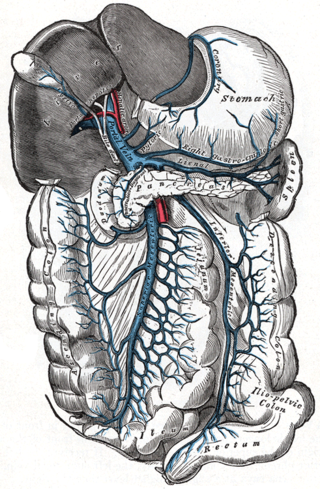
Portal hypertension is defined as increased portal venous pressure, with a hepatic venous pressure gradient greater than 5 mmHg. Normal portal pressure is 1–4 mmHg; clinically insignificant portal hypertension is present at portal pressures 5–9 mmHg; clinically significant portal hypertension is present at portal pressures greater than 10 mmHg. The portal vein and its branches supply most of the blood and nutrients from the intestine to the liver.

Gastrointestinal bleeding, also called gastrointestinal hemorrhage (GIB), is all forms of bleeding in the gastrointestinal tract, from the mouth to the rectum. When there is significant blood loss over a short time, symptoms may include vomiting red blood, vomiting black blood, bloody stool, or black stool. Small amounts of bleeding over a long time may cause iron-deficiency anemia resulting in feeling tired or heart-related chest pain. Other symptoms may include abdominal pain, shortness of breath, pale skin, or passing out. Sometimes in those with small amounts of bleeding no symptoms may be present.

Gastric varices are dilated submucosal veins in the lining of the stomach, which can be a life-threatening cause of bleeding in the upper gastrointestinal tract. They are most commonly found in patients with portal hypertension, or elevated pressure in the portal vein system, which may be a complication of cirrhosis. Gastric varices may also be found in patients with thrombosis of the splenic vein, into which the short gastric veins that drain the fundus of the stomach flow. The latter may be a complication of acute pancreatitis, pancreatic cancer, or other abdominal tumours, as well as hepatitis C. Gastric varices and associated bleeding are a potential complication of schistosomiasis resulting from portal hypertension.

Transjugular intrahepatic portosystemic shunt is an artificial channel within the liver that establishes communication between the inflow portal vein and the outflow hepatic vein. It is used to treat portal hypertension which frequently leads to intestinal bleeding, life-threatening esophageal bleeding and the buildup of fluid within the abdomen (ascites).

Portal vein thrombosis (PVT) is a vascular disease of the liver that occurs when a blood clot occurs in the hepatic portal vein, which can lead to increased pressure in the portal vein system and reduced blood supply to the liver. The mortality rate is approximately 1 in 10.

In medicine, a distal splenorenal shunt procedure (DSRS), also splenorenal shunt procedure and Warren shunt, is a surgical procedure in which the distal splenic vein is attached to the left renal vein. It is used to treat portal hypertension and its main complication. It was developed by W. Dean Warren.

A Sengstaken–Blakemore tube is a medical device inserted through the nose or mouth and used occasionally in the management of upper gastrointestinal hemorrhage due to esophageal varices. The use of the tube was originally described in 1950, although similar approaches to bleeding varices were described by Westphal in 1930. With the advent of modern endoscopic techniques which can rapidly and definitively control variceal bleeding, Sengstaken–Blakemore tubes are rarely used at present.
A portacaval anastomosis or portocaval anastomosis is a specific type of circulatory anastomosis that occurs between the veins of the portal circulation and the vena cava, thus forming one of the principal types of portasystemic anastomosis or portosystemic anastomosis, as it connects the portal circulation to the systemic circulation, providing an alternative pathway for the blood. When there is a blockage of the portal system, portocaval anastomosis enables the blood to still reach the systemic venous circulation. The inferior end of the esophagus and the superior part of the rectum are potential sites of a harmful portocaval anastomosis.
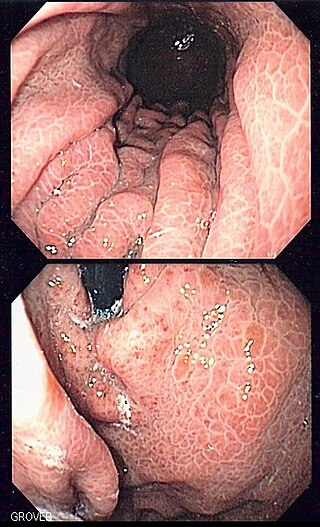
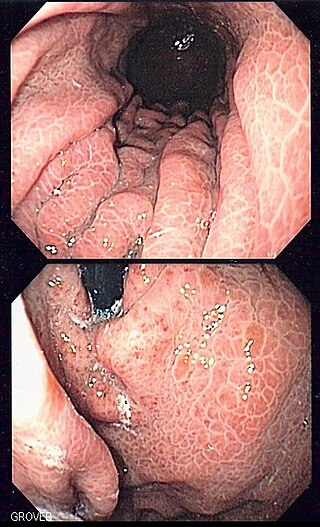
Portal hypertensive gastropathy refers to changes in the mucosa of the stomach in patients with portal hypertension; by far the most common cause of this is cirrhosis of the liver. These changes in the mucosa include friability of the mucosa and the presence of ectatic blood vessels at the surface. Patients with portal hypertensive gastropathy may experience bleeding from the stomach, which may uncommonly manifest itself in vomiting blood or melena; however, portal hypertension may cause several other more common sources of upper gastrointestinal bleeding, such as esophageal varices and gastric varices. On endoscopic evaluation of the stomach, this condition shows a characteristic mosaic or "snake-skin" appearance to the mucosa of the stomach.
Portal venous pressure is the blood pressure in the hepatic portal vein, and is normally between 5-10 mmHg. Raised portal venous pressure is termed portal hypertension, and has numerous sequelae such as ascites and hepatic encephalopathy.

n-Butyl cyanoacrylate, a cyanoacrylate ester, is a butyl ester of 2-cyano-2-propenoic acid. It is a colorless liquid with a sharp, irritating odor. It is insoluble in water. Its chief use is as the main component of medical cyanoacrylate glues. It can be encountered under various trade names, e.g. Cutseal, MediBond, MediCryl, PeriAcryl, GluStitch, Xoin, Gesika, VetGlu, Vetbond, LiquiVet, Indermil, LiquiBand, Histoacryl, IFABond, CutisSeal and others. The generic international nonproprietary name (INN) for NBCA is enbucrilate.
Therapeutic endoscopy is the medical term for an endoscopic procedure during which treatment is carried out via the endoscope. This contrasts with diagnostic endoscopy, where the aim of the procedure is purely to visualize a part of the gastrointestinal, respiratory or urinary tract in order to aid diagnosis. In practice, a procedure which starts as a diagnostic endoscopy may become a therapeutic endoscopy depending on the findings, such as in cases of upper gastrointestinal bleeding, or the finding of polyps during colonoscopy.

Cirrhosis, also known as liver cirrhosis or hepatic cirrhosis, and end-stage liver disease, is the impaired liver function caused by the formation of scar tissue known as fibrosis due to damage caused by liver disease. Damage to the liver leads to repair of liver tissue and subsequent formation of scar tissue. Over time, scar tissue can replace normal functioning tissue, leading to the impaired liver function of cirrhosis. The disease typically develops slowly over months or years. Early symptoms may include tiredness, weakness, loss of appetite, unexplained weight loss, nausea and vomiting, and discomfort in the right upper quadrant of the abdomen. As the disease worsens, symptoms may include itchiness, swelling in the lower legs, fluid build-up in the abdomen, jaundice, bruising easily, and the development of spider-like blood vessels in the skin. The fluid build-up in the abdomen may develop into spontaneous infections. More serious complications include hepatic encephalopathy, bleeding from dilated veins in the esophagus, stomach, or intestines, and liver cancer.
Anorectal varices are the dilation of collateral submucosal vessels due to backflow in the veins of the rectum. Typically this occurs due to portal hypertension which shunts venous blood from the portal system through the portosystemic anastomosis present at this site into the systemic venous system. This can also occur in the esophagus, causing esophageal varices, and at the level of the umbilicus, causing caput medusae. Between 44% and 78% of patients with portal hypertension get anorectal varices.
The Sugiura procedure is a surgical technique that involves the removal and transection of the blood vessels that supply the upper portion of the stomach and the esophagus. The procedure also involves a splenectomy. The operation was originally developed to treat bleeding esophageal varices that were untreatable by other conventional methods. It was originally developed as a two-step operation, but has been modified numerous times by many surgeons since its original creation.
Balloon-occluded retrograde transvenous obliteration (BRTO) is an endovascular procedure used for the treatment of gastric varices. When performing the procedure, an interventional radiologist accesses blood vessels using a catheter, inflates a balloon and injects a substance into the variceal blood vessels that causes blockage of those vessels. To prevent the flow of the agent out of the intended site, a balloon is inflated during the procedure, which occludes.