A Krukenberg tumor refers to a malignancy in the ovary that metastasized from a primary site, classically the gastrointestinal tract, although it can arise in other tissues such as the breast. Gastric adenocarcinoma, especially at the pylorus, is the most common source. Krukenberg tumors are often found in both ovaries, consistent with its metastatic nature.

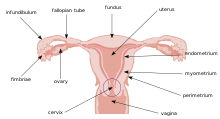
Ovarian cancer is a cancerous tumor of an ovary. It may originate from the ovary itself or more commonly from communicating nearby structures such as fallopian tubes or the inner lining of the abdomen. The ovary is made up of three different cell types including epithelial cells, germ cells, and stromal cells. When these cells become abnormal, they have the ability to divide and form tumors. These cells can also invade or spread to other parts of the body. When this process begins, there may be no or only vague symptoms. Symptoms become more noticeable as the cancer progresses. These symptoms may include bloating, vaginal bleeding, pelvic pain, abdominal swelling, constipation, and loss of appetite, among others. Common areas to which the cancer may spread include the lining of the abdomen, lymph nodes, lungs, and liver.

A serous tumour is a neoplasm that typically has papillary to solid formations of tumor cells with crowded nuclei, and which typically arises on the modified Müllerian-derived serous membranes that surround the ovaries in females. Such ovarian tumors are part of the surface epithelial-stromal tumour group of ovarian tumors. They are common neoplasms with a strong tendency to occur bilaterally, and they account for approximately a quarter of all ovarian tumors.

Surface epithelial-stromal tumors are a class of ovarian neoplasms that may be benign or malignant. Neoplasms in this group are thought to be derived from the ovarian surface epithelium or from ectopic endometrial or fallopian tube (tubal) tissue. Tumors of this type are also called ovarian adenocarcinoma. This group of tumors accounts for 90% to 95% of all cases of ovarian cancer; however is mainly only found in postmenopausal women with the exception of the United States where 7% of cases occur in women under the age of 40. Serum CA-125 is often elevated but is only 50% accurate so it is not a useful tumor marker to assess the progress of treatment. 75% of women with epithelial ovarian cancer are found within the advanced-stages; however younger patients are more likely to have better prognoses than older patients.

Gynecologic ultrasonography or gynecologic sonography refers to the application of medical ultrasonography to the female pelvic organs as well as the bladder, the adnexa, and the recto-uterine pouch. The procedure may lead to other medically relevant findings in the pelvis.This technique is useful to detect myomas or mullerian malformations.

Pseudomyxoma peritonei (PMP) is a clinical condition caused by cancerous cells that produce abundant mucin or gelatinous ascites. The tumors cause fibrosis of tissues and impede digestion or organ function, and if left untreated, the tumors and mucin they produce will fill the abdominal cavity. This will result in compression of organs and will destroy the function of the colon, small intestine, stomach, or other organs. Prognosis with treatment in many cases is optimistic, but the disease is lethal if untreated, with death occurring via cachexia, bowel obstruction, or other types of complications.
In medicine, Meigs's syndrome, also Meigs syndrome or Demons–Meigs syndrome, is the triad of ascites, pleural effusion, and benign ovarian tumor. Meigs syndrome resolves after the resection of the tumor. Because the transdiaphragmatic lymphatic channels are larger in diameter on the right, the pleural effusion is classically on the right side. The causes of the ascites and pleural effusion are poorly understood. Atypical Meigs syndrome, characterized by a benign pelvic mass with right-sided pleural effusion but without ascites, can also occur. As in typical Meigs syndrome, pleural effusion resolves after removal of the pelvic mass.

Primary peritoneal cancer or carcinoma is also known as serous surface papillary carcinoma, primary peritoneal carcinoma, extra-ovarian serous carcinoma, primary serous papillary carcinoma, and psammomacarcinoma. It was historically classified under "carcinoma of unknown primary" (CUP). Primary peritoneal cancer is a cancer of the cells lining the peritoneum, or abdominal cavity. It usually affects women and is diagnosed after the age of 60; it very rarely affects men.

A hydrosalpinx is a condition that occurs when a fallopian tube is blocked and fills with serous or clear fluid near the ovary. The blocked tube may become substantially distended giving the tube a characteristic sausage-like or retort-like shape. The condition is often bilateral and the affected tubes may reach several centimeters in diameter. The blocked tubes cause infertility. A fallopian tube filled with blood is a hematosalpinx, and with pus a pyosalpinx.

An adnexal mass is a lump in the tissue of the adnexa of the uterus. Adnexal masses can be benign (noncancerous) or malignant (cancerous), and they can be categorized as simple or complex.

Uterine serous carcinoma is a malignant form of serous tumor that originates in the uterus. It is an uncommon form of endometrial cancer that typically arises in postmenopausal women. It is typically diagnosed on endometrial biopsy, prompted by post-menopausal bleeding.
A borderline tumor, sometimes called low malignant potential (LMP) tumor, is a distinct but yet heterogeneous group of tumors defined by their histopathology as atypical epithelial proliferation without stromal invasion. It generally refers to such tumors in the ovary but borderline tumors may rarely occur at other locations as well.

Endosalpingiosis is a condition in which fallopian tube-like epithelium is found outside the fallopian tube. It is unknown what causes this condition. It is generally accepted that the condition develops from transformation of coelomic tissue. It is often an incidental finding and is not usually associated with any pathology.

Ovarian serous cystadenoma, also known as serous cystadenoma, is the most common ovarian neoplasm, representing 20% of ovarian neoplasms, and is benign.

Adenosarcoma is a rare malignant tumor that occurs in women of all age groups, but most commonly post-menopause. Adenosarcoma arises from mesenchymal tissue and has a mixture of the tumoral components of an adenoma, a tumor of epithelial origin, and a sarcoma, a tumor originating from connective tissue. The adenoma, or epithelial component of the tumor, is benign, while the sarcomatous stroma is malignant. The most common site of adenosarcoma formation is the uterus, but it can also occur in the cervix and ovaries. It more rarely arises in the vagina and fallopian tubes as well as primary pelvic or peritoneal sites, such as the omentum, especially in those with a history of endometriosis. The rare cases of adenosarcoma outside the female genital tract usually occur in the liver, bladder, kidney, as well as the intestine and are typically associated with endometriosis.

Paraovarian cysts or paratubal cysts are epithelium-lined fluid-filled cysts in the adnexa adjacent to the fallopian tube and ovary. The terms are used interchangeably, and depend on the location of the cyst.
High-grade serous carcinoma (HGSC) is a type of tumour that arises from the serous epithelial layer in the abdominopelvic cavity and is mainly found in the ovary. HGSCs make up the majority of ovarian cancer cases and have the lowest survival rates. HGSC is distinct from low-grade serous carcinoma (LGSC) which arises from ovarian tissue, is less aggressive and is present in stage I ovarian cancer where tumours are localised to the ovary.
Ovarian germ cell tumors (OGCTs) are heterogeneous tumors that are derived from the primitive germ cells of the embryonic gonad, which accounts for about 2.6% of all ovarian malignancies. There are four main types of OGCTs, namely dysgerminomas, yolk sac tumor, teratoma, and choriocarcinoma.

The SEE-FIM protocol is a pathology dissection protocol for Sectioning and Extensively Examining the Fimbria (SEE-FIM). This protocol is intended to provide for the optimal microscopic examination of the distal fallopian tube (fimbria) to identify either cancerous or precancerous conditions in this organ.

Ovarian squamous cell carcinoma (oSCC) or squamous ovarian carcinoma (SOC) is a rare tumor that accounts for 1% of ovarian cancers. Included in the World Health Organization's classification of ovarian cancer, it mainly affects women above 45 years of age. Survival depends on how advanced the disease is and how different or similar the individual cancer cells are.