Metastasis is a pathogenic agent's spread from an initial or primary site to a different or secondary site within the host's body; the term is typically used when referring to metastasis by a cancerous tumor. The newly pathological sites, then, are metastases (mets). It is generally distinguished from cancer invasion, which is the direct extension and penetration by cancer cells into neighboring tissues.

Carcinoma is a malignancy that develops from epithelial cells. Specifically, a carcinoma is a cancer that begins in a tissue that lines the inner or outer surfaces of the body, and that arises from cells originating in the endodermal, mesodermal or ectodermal germ layer during embryogenesis.

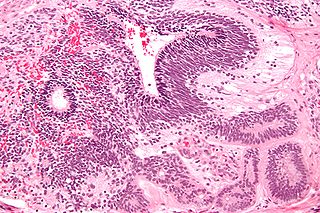
Endometrial cancer is a cancer that arises from the endometrium. It is the result of the abnormal growth of cells that have the ability to invade or spread to other parts of the body. The first sign is most often vaginal bleeding not associated with a menstrual period. Other symptoms include pain with urination, pain during sexual intercourse, or pelvic pain. Endometrial cancer occurs most commonly after menopause.

Ovarian cancer is a cancerous tumor of an ovary. It may originate from the ovary itself or more commonly from communicating nearby structures such as fallopian tubes or the inner lining of the abdomen. The ovary is made up of three different cell types including epithelial cells, germ cells, and stromal cells. When these cells become abnormal, they have the ability to divide and form tumors. These cells can also invade or spread to other parts of the body. When this process begins, there may be no or only vague symptoms. Symptoms become more noticeable as the cancer progresses. These symptoms may include bloating, vaginal bleeding, pelvic pain, abdominal swelling, constipation, and loss of appetite, among others. Common areas to which the cancer may spread include the lining of the abdomen, lymph nodes, lungs, and liver.

A serous tumour is a neoplasm that typically has papillary to solid formations of tumor cells with crowded nuclei, and which typically arises on the modified Müllerian-derived serous membranes that surround the ovaries in females. Such ovarian tumors are part of the surface epithelial-stromal tumour group of ovarian tumors. They are common neoplasms with a strong tendency to occur bilaterally, and they account for approximately a quarter of all ovarian tumors.

Surface epithelial-stromal tumors are a class of ovarian neoplasms that may be benign or malignant. Neoplasms in this group are thought to be derived from the ovarian surface epithelium or from ectopic endometrial or fallopian tube (tubal) tissue. Tumors of this type are also called ovarian adenocarcinoma. This group of tumors accounts for 90% to 95% of all cases of ovarian cancer; however is mainly only found in postmenopausal women with the exception of the United States where 7% of cases occur in women under the age of 40. Serum CA-125 is often elevated but is only 50% accurate so it is not a useful tumor marker to assess the progress of treatment. 75% of women with epithelial ovarian cancer are found within the advanced-stages; however younger patients are more likely to have better prognoses than older patients.

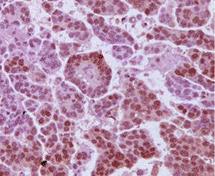
Sex cord–gonadal stromal tumour is a group of tumours derived from the stromal component of the ovary and testis, which comprises the granulosa, thecal cells and fibrocytes. In contrast, the epithelial cells originate from the outer epithelial lining surrounding the gonad while the germ cell tumors arise from the precursor cells of the gametes, hence the name germ cell. In humans, this group accounts for 8% of ovarian cancers and under 5% of testicular cancers. Their diagnosis is histological: only a biopsy of the tumour can make an exact diagnosis. They are often suspected of being malignant prior to operation, being solid ovarian tumours that tend to occur most commonly in post menopausal women.
In medicine, Meigs's syndrome, also Meigs syndrome or Demons–Meigs syndrome, is the triad of ascites, pleural effusion, and benign ovarian tumor. Meigs syndrome resolves after the resection of the tumor. Because the transdiaphragmatic lymphatic channels are larger in diameter on the right, the pleural effusion is classically on the right side. The causes of the ascites and pleural effusion are poorly understood. Atypical Meigs syndrome, characterized by a benign pelvic mass with right-sided pleural effusion but without ascites, can also occur. As in typical Meigs syndrome, pleural effusion resolves after removal of the pelvic mass.

A carcinoid is a slow-growing type of neuroendocrine tumor originating in the cells of the neuroendocrine system. In some cases, metastasis may occur. Carcinoid tumors of the midgut are associated with carcinoid syndrome.

Ovarian tumors, or ovarian neoplasms, are tumors found in the ovary. They can be benign or malignant. They consist of mainly solid tissue, while ovarian cysts contain fluid.
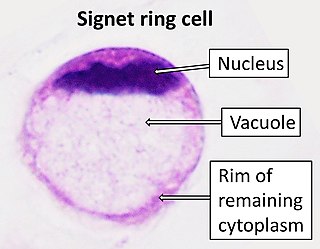
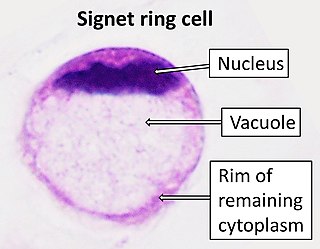
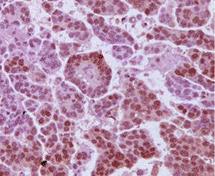
Signet ring cell carcinoma (SRCC) is a rare form of highly malignant adenocarcinoma that produces mucin. It is an epithelial malignancy characterized by the histologic appearance of signet ring cells.
An immature teratoma is a teratoma that contains anaplastic immature elements, and is often synonymous with malignant teratoma. A teratoma is a tumor of germ cell origin, containing tissues from more than one germ cell line, It can be ovarian or testicular in its origin. and are almost always benign. An immature teratoma is thus a very rare tumor, representing 1% of all teratomas, 1% of all ovarian cancers, and 35.6% of malignant ovarian germ cell tumors. It displays a specific age of incidence, occurring most frequently in the first two decades of life and almost never after menopause. Unlike a mature cystic teratoma, an immature teratoma contains immature or embryonic structures. It can coexist with mature cystic teratomas and can constitute of a combination of both adult and embryonic tissue. The most common symptoms noted are abdominal distension and masses. Prognosis and treatment options vary and largely depend on grade, stage and karyotype of the tumor itself.

Primary fallopian tube cancer (PFTC), also known as tubal cancer, is a malignant neoplasm that originates from the fallopian tube. Along with primary ovarian and peritoneal carcinomas, it is grouped under epithelial ovarian cancers; cancers of the ovary that originate from a fallopian tube precursor.

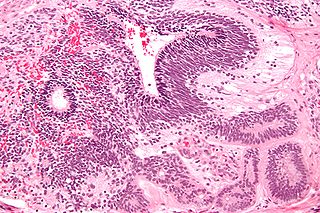
Adenosarcoma is a rare malignant tumor that occurs in women of all age groups, but most commonly post-menopause. Adenosarcoma arises from mesenchymal tissue and has a mixture of the tumoral components of an adenoma, a tumor of epithelial origin, and a sarcoma, a tumor originating from connective tissue. The adenoma, or epithelial component of the tumor, is benign, while the sarcomatous stroma is malignant. The most common site of adenosarcoma formation is the uterus, but it can also occur in the cervix and ovaries. It more rarely arises in the vagina and fallopian tubes as well as primary pelvic or peritoneal sites, such as the omentum, especially in those with a history of endometriosis. The rare cases of adenosarcoma outside the female genital tract usually occur in the liver, bladder, kidney, as well as the intestine and are typically associated with endometriosis.

The International Ovarian Tumor Analysis (IOTA) group was formed in 1999 by Dirk Timmerman, Tom Bourne, and Lil Valentin. Its first aim was to develop standardised terminology, and in 2000 IOTA published a consensus statement on terms, definitions and measurements to describe the sonographic features of adnexal masses that is now widely used today. IOTA now comprises one of a portfolio of studies examining many aspects of gynaecological ultrasonography and early pregnancy within a network of contributing centres throughout the world that are coordinated from KU Leuven
High-grade serous carcinoma (HGSC) is a type of tumour that arises from the serous epithelial layer in the abdominopelvic cavity and is mainly found in the ovary. HGSCs make up the majority of ovarian cancer cases and have the lowest survival rates. HGSC is distinct from low-grade serous carcinoma (LGSC) which arises from ovarian tissue, is less aggressive and is present in stage I ovarian cancer where tumours are localised to the ovary.
Ovarian germ cell tumors (OGCTs) are heterogeneous tumors that are derived from the primitive germ cells of the embryonic gonad, which accounts for about 2.6% of all ovarian malignancies. There are four main types of OGCTs, namely dysgerminomas, yolk sac tumor, teratoma, and choriocarcinoma.
Bradley J. Monk is an American gynecologic oncologist, academician and researcher. He is a Professor on the Clinical Scholar Track in the Department of Obstetrics and Gynecology at the University of Arizona College of Medicine in Phoenix, Arizona, as well as at the Creighton University School of Medicine in Omaha, Nebraska. He also serves as Director of the Division of Gynecologic Oncology at the St. Joseph's Hospital and Medical Center in Phoenix.

The SEE-FIM protocol is a pathology dissection protocol for Sectioning and Extensively Examining the Fimbria (SEE-FIM). This protocol is intended to provide for the optimal microscopic examination of the distal fallopian tube (fimbria) to identify either cancerous or precancerous conditions in this organ.

Ovarian squamous cell carcinoma (oSCC) or squamous ovarian carcinoma (SOC) is a rare tumor that accounts for 1% of ovarian cancers. Included in the World Health Organization's classification of ovarian cancer, it mainly affects women above 45 years of age. Survival depends on how advanced the disease is and how different or similar the individual cancer cells are.