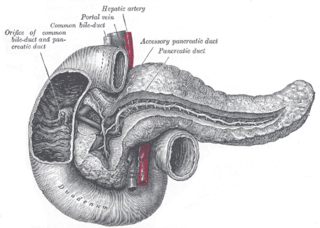
The pancreas is an organ of the digestive system and endocrine system of vertebrates. In humans, it is located in the abdomen behind the stomach and functions as a gland. The pancreas is a mixed or heterocrine gland, i.e., it has both an endocrine and a digestive exocrine function. 99% of the pancreas is exocrine and 1% is endocrine. As an endocrine gland, it functions mostly to regulate blood sugar levels, secreting the hormones insulin, glucagon, somatostatin and pancreatic polypeptide. As a part of the digestive system, it functions as an exocrine gland secreting pancreatic juice into the duodenum through the pancreatic duct. This juice contains bicarbonate, which neutralizes acid entering the duodenum from the stomach; and digestive enzymes, which break down carbohydrates, proteins and fats in food entering the duodenum from the stomach.

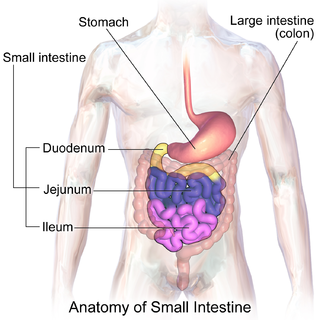
The duodenum is the first section of the small intestine in most higher vertebrates, including mammals, reptiles, and birds. In mammals it may be the principal site for iron absorption. The duodenum precedes the jejunum and ileum and is the shortest part of the small intestine.
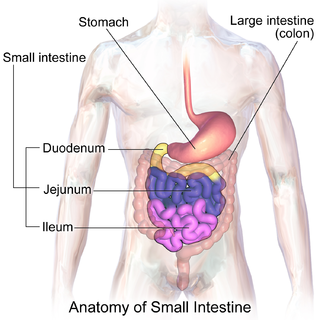
The small intestine or small bowel is an organ in the gastrointestinal tract where most of the absorption of nutrients from food takes place. It lies between the stomach and large intestine, and receives bile and pancreatic juice through the pancreatic duct to aid in digestion. The small intestine is about 5.5 metres long and folds many times to fit in the abdomen. Although it is longer than the large intestine, it is called the small intestine because it is narrower in diameter.

A bile duct is any of a number of long tube-like structures that carry bile, and is present in most vertebrates. The bile duct is separated into three main parts: the fundus (superior), the body (middle), and the neck (inferior).

Endoscopic retrograde cholangiopancreatography (ERCP) is a technique that combines the use of endoscopy and fluoroscopy to diagnose and treat certain problems of the biliary or pancreatic ductal systems. It is primarily performed by highly skilled and specialty trained gastroenterologists. Through the endoscope, the physician can see the inside of the stomach and duodenum, and inject a contrast medium into the ducts in the biliary tree and pancreas so they can be seen on radiographs.

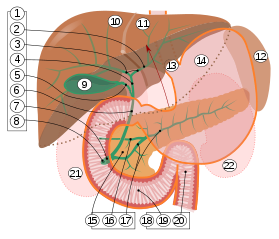
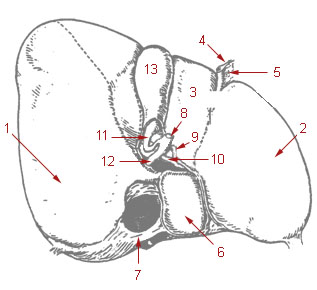
The bile duct is a part of the biliary tract. It is formed by the union of the common hepatic duct and cystic duct. It ends by uniting with the pancreatic duct to form the hepatopancreatic ampulla. It possesses its own sphincter to enable regulation of bile flow.
The cystic duct is the duct that (typically) joins the gallbladder and the common hepatic duct; the union of the cystic duct and common hepatic duct forms the bile duct. Its length varies. It is often tortuous.

Digestive enzymes are a group of enzymes that break down polymeric macromolecules into their smaller building blocks, in order to facilitate their absorption into the cells of the body. Digestive enzymes are found in the digestive tracts of animals and in the tracts of carnivorous plants, where they aid in the digestion of food, as well as inside cells, especially in their lysosomes, where they function to maintain cellular survival. Digestive enzymes of diverse specificities are found in the saliva secreted by the salivary glands, in the secretions of cells lining the stomach, in the pancreatic juice secreted by pancreatic exocrine cells, and in the secretions of cells lining the small and large intestines.
The common hepatic duct is the first part of the biliary tract. It joins the cystic duct coming from the gallbladder to form the common bile duct.
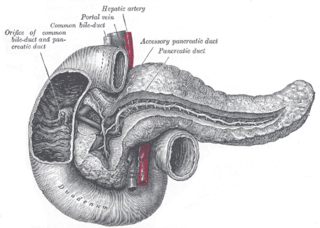
The pancreatic duct or duct of Wirsung is a duct joining the pancreas to the common bile duct. This supplies it with pancreatic juice from the exocrine pancreas, which aids in digestion.

The ampulla of Vater, hepatopancreatic ampulla or hepatopancreatic duct is the common duct that is usually formed by a union of the common bile duct and the pancreatic duct within the wall of the duodenum. This common duct usually features a dilation ("ampulla"). The common duct then opens medially into the descending part of the duodenum at the major duodenal papilla. The common duct usually measures 2-10mm in length.

Ascending cholangitis, also known as acute cholangitis or simply cholangitis, is inflammation of the bile duct, usually caused by bacteria ascending from its junction with the duodenum. It tends to occur if the bile duct is already partially obstructed by gallstones.

The biliary tract refers to the liver, gallbladder and bile ducts, and how they work together to make, store and secrete bile. Bile consists of water, electrolytes, bile acids, cholesterol, phospholipids and conjugated bilirubin. Some components are synthesized by hepatocytes ; the rest are extracted from the blood by the liver.

Percutaneous transhepatic cholangiography, percutaneous hepatic cholangiogram (PTHC) is a radiological technique used to visualize the anatomy of the biliary tract. A contrast medium is injected into a bile duct in the liver, after which X-rays are taken. It allows access to the biliary tree in cases where endoscopic retrograde cholangiopancreatography has been unsuccessful. Initially reported in 1937, the procedure became popular in 1952.
The minor duodenal papilla is the opening of the accessory pancreatic duct into the descending second section of the duodenum.

Sphincter of Oddi dysfunction refers to a group of functional disorders leading to abdominal pain due to dysfunction of the Sphincter of Oddi: functional biliary sphincter of Oddi and functional pancreatic sphincter of Oddi disorder. The sphincter of Oddi is a sphincter muscle, a circular band of muscle at the bottom of the biliary tree which controls the flow of pancreatic juices and bile into the second part of the duodenum. The pathogenesis of this condition is recognized to encompass stenosis or dyskinesia of the sphincter of Oddi ; consequently the terms biliary dyskinesia, papillary stenosis, and postcholecystectomy syndrome have all been used to describe this condition. Both stenosis and dyskinesia can obstruct flow through the sphincter of Oddi and can therefore cause retention of bile in the biliary tree and pancreatic juice in the pancreatic duct.

The human digestive system consists of the gastrointestinal tract plus the accessory organs of digestion. Digestion involves the breakdown of food into smaller and smaller components, until they can be absorbed and assimilated into the body. The process of digestion has three stages: the cephalic phase, the gastric phase, and the intestinal phase.

The sphincter of Oddi, abbreviated as SO, is a muscular valve that in some animals, including humans, controls the flow of bile and pancreatic juice out of the gallbladder and pancreas respectively through the ampulla of Vater into the second part of the duodenum. It is named after Ruggero Oddi.

Biliary endoscopic sphincterotomy is a procedure where the sphincter of Oddi and the segment of the common bile duct where it enters the duodenum are cannulated and then cut with a sphincterotome, a device that includes a wire which cuts with an electric current (electrocautery).
The sphincter of Boyden is a sphincter located in the common bile duct before it joins with the pancreatic duct to form the ampulla of vater. This sphincter controls the flow of bile into the pancreatic duct and it helps in filling up of the gallbladder with bile.