The vagina is a tubular musculo-mucosal reproductive organ that is part of the female reproductive system. In mammals, it connects the vulva to the uterus. In birds and reptiles, it connects the uterus to the cloaca. In insects and other invertebrates, the vagina is the terminal part of the oviduct. It is involved during copulation and, in mammals, during parturition.

The Papanicolaou test is a method of cervical screening used to detect potentially precancerous and cancerous processes in the cervix or, more rarely, anus. Abnormal findings are often followed up by more sensitive diagnostic procedures and, if warranted, interventions that aim to prevent progression to cervical cancer. The test was independently invented in the 1920s by the Greek physician Georgios Papanikolaou and named after him. A simplified version of the test was introduced by the Canadian obstetrician Anna Marion Hilliard in 1957.
Obstetrics and gynaecology is the medical specialty that encompasses the two subspecialties of obstetrics and gynaecology. The specialization is an important part of care for women's health.

Gynaecology or gynecology is the area of medicine that involves the treatment of women's diseases, especially those of the reproductive organs. It is often paired with the field of obstetrics, forming the combined area of obstetrics and gynaecology (OB-GYN).
Dyspareunia is painful sexual intercourse due to medical or psychological causes. The term dyspareunia covers both female dyspareunia and male dyspareunia, but many discussions that use the term without further specification concern the female type, which is more common than the male type. In females, the pain can primarily be on the external surface of the genitalia, or deeper in the pelvis upon deep pressure against the cervix. Medically, dyspareunia is a pelvic floor dysfunction and is frequently underdiagnosed. It can affect a small portion of the vulva or vagina or be felt all over the surface. Understanding the duration, location, and nature of the pain is important in identifying the causes of the pain.

A speculum is a medical tool for investigating body orifices, with a form dependent on the orifice for which it is designed. In old texts, the speculum may also be referred to as a diopter or dioptra. Like an endoscope, a speculum allows a view inside the body; endoscopes, however, tend to have optics while a speculum is intended for direct vision.

Cervicitis is inflammation of the uterine cervix. Cervicitis in women has many features in common with urethritis in men and many cases are caused by sexually transmitted infections. Non-infectious causes of cervicitis can include intrauterine devices, contraceptive diaphragms, and allergic reactions to spermicides or latex condoms. Cervicitis affects over half of all women during their adult life.

Pelvic floor dysfunction is a term used for a variety of disorders that occur when pelvic floor muscles and ligaments are impaired. The condition affects up to 50 percent of women who have given birth. Although this condition predominantly affects women, up to 16 percent of men are affected as well. Symptoms can include pelvic pain, pressure, pain during sex, urinary incontinence (UI), overactive bladder, bowel incontinence, incomplete emptying of feces, constipation, myofascial pelvic pain and pelvic organ prolapse. When pelvic organ prolapse occurs, there may be visible organ protrusion or a lump felt in the vagina or anus. Research carried out in the UK has shown that symptoms can restrict everyday life for women. However, many people found it difficult to talk about it and to seek care, as they experienced embarrassment and stigma.

Vaginal bleeding is any expulsion of blood from the vagina. This bleeding may originate from the uterus, vaginal wall, or cervix. Generally, it is either part of a normal menstrual cycle or is caused by hormonal or other problems of the reproductive system, such as abnormal uterine bleeding.

Vaginal discharge is a mixture of liquid, cells, and bacteria that lubricate and protect the vagina. This mixture is constantly produced by the cells of the vagina and cervix, and it exits the body through the vaginal opening. The composition, amount, and quality of discharge varies between individuals and can vary throughout the menstrual cycle and throughout the stages of sexual and reproductive development. Normal vaginal discharge may have a thin, watery consistency or a thick, sticky consistency, and it may be clear or white in color. Normal vaginal discharge may be large in volume but typically does not have a strong odor, nor is it typically associated with itching or pain. While most discharge is considered physiologic or represents normal functioning of the body, some changes in discharge can reflect infection or other pathological processes. Infections that may cause changes in vaginal discharge include vaginal yeast infections, bacterial vaginosis, and sexually transmitted infections. The characteristics of abnormal vaginal discharge vary depending on the cause, but common features include a change in color, a foul odor, and associated symptoms such as itching, burning, pelvic pain, or pain during sexual intercourse.

Uterine prolapse is a form of pelvic organ prolapse in which the uterus and a portion of the upper vagina protrude into the vaginal canal and, in severe cases, through the opening of the vagina. It is most often caused by injury or damage to structures that hold the uterus in place within the pelvic cavity. Symptoms may include vaginal fullness, pain with sexual intercourse, difficulty urinating, and urinary incontinence. Risk factors include older age, pregnancy, vaginal childbirth, obesity, chronic constipation, and chronic cough. Prevalence, based on physical exam alone, is estimated to be approximately 14%.

The endometrial biopsy is a medical procedure that involves taking a tissue sample of the lining of the uterus. The tissue subsequently undergoes a histologic evaluation which aids the physician in forming a diagnosis.

Hematometra is a medical condition involving collection or retention of blood in the uterus. It is most commonly caused by an imperforate hymen or a transverse vaginal septum.
Neuroendocrine carcinoma of the cervix is best defined separately:Neuroendocrine: Of, relating to, or involving the interaction between the nervous system and the hormones of the endocrine glands.Carcinoma: An invasive malignant tumor derived from epithelial tissue that tends to metastasize to other areas of the body.

Fertility testing is the process by which fertility is assessed, both generally and also to find the "fertile window" in the menstrual cycle. General health affects fertility, and STI testing is an important related field.
A well-woman examination is an exam offered to women to review elements of their reproductive health. The exam includes a breast examination, a pelvic examination and a Pap smear but may include other procedures. Hospitals employ strict policies relating to the provision of consent by the patient, the availability of chaperones at the examination, and the absence of other parties.

Postcoital bleeding (PCB) is non-menstrual vaginal bleeding that occurs during or after sexual intercourse. Though some causes are with associated pain, it is typically painless and frequently associated with intermenstrual bleeding.
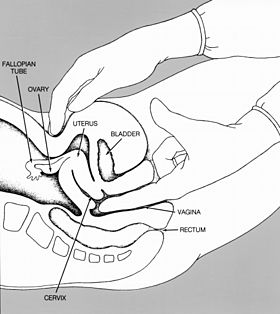
A rectovaginal examination is a type of gynecological examination used to supplement a pelvic examination. In the rectovaginal examination, a doctor or other health care provider places one finger in the vagina and another in the rectum to assess the rectovaginal septum. The examiner will look for any scarring or masses that may indicate cancer or another disease. Typically, a rectovaginal examination is performed to assess pelvic pain, rectal symptoms, or a pelvic mass. It can also provide a sample for fecal occult blood testing.
Pediatric gynaecology or pediatric gynecology is the medical practice dealing with the health of the vagina, vulva, uterus, and ovaries of infants, children, and adolescents. Its counterpart is pediatric andrology, which deals with medical issues specific to the penis and testes.

Squamous cell carcinoma of the vagina is a potentially invasive type of cancer that forms in the tissues of the vagina. Though uncommonly diagnosed, squamous cell cancer of the vagina (SCCV) is the most common type of vaginal cancer, accounting for 80-90% of cases as well as 2% of all gynecological cancers. SCCV forms in squamous cells, which are the thin, flat cells lining the vagina. SCCV initially spreads superficially within the vaginal wall and can slowly spread to invade other vaginal tissues. Because of its slow growth, this cancer may cause no symptoms, or it may present with signs like irregular bleeding, pain, or a vaginal mass. This carcinoma can metastasize to the lungs or less frequently to the liver, bone, or other sites. SCCV has many risk factors in common with cervical cancer and is similarly strongly associated with infection with oncogenic strains of human papillomavirus (HPV). Diagnosis of SCCV is done by pelvic exam and biopsy of the tissue. Treatment and prognosis will depend on the stage, location, and characteristics of the cancer.