In biology, homeostasis is the state of steady internal, physical, and chemical conditions maintained by living systems. This is the condition of optimal functioning for the organism and includes many variables, such as body temperature and fluid balance, being kept within certain pre-set limits. Other variables include the pH of extracellular fluid, the concentrations of sodium, potassium and calcium ions, as well as that of the blood sugar level, and these need to be regulated despite changes in the environment, diet, or level of activity. Each of these variables is controlled by one or more regulators or homeostatic mechanisms, which together maintain life.

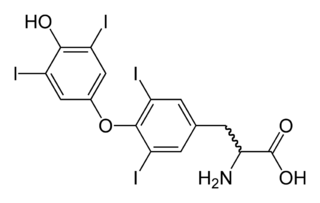
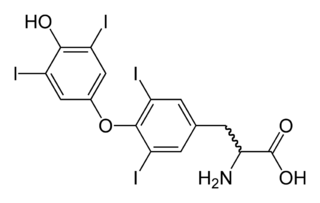
The thyroid, or thyroid gland, is an endocrine gland in vertebrates. In humans it is in the neck and consists of two connected lobes. The lower two thirds of the lobes are connected by a thin band of tissue called the thyroid isthmus. The thyroid is located at the front of the neck, below the Adam's apple. Microscopically, the functional unit of the thyroid gland is the spherical thyroid follicle, lined with follicular cells (thyrocytes), and occasional parafollicular cells that surround a lumen containing colloid. The thyroid gland secretes three hormones: the two thyroid hormones – triiodothyronine (T3) and thyroxine (T4) – and a peptide hormone, calcitonin. The thyroid hormones influence the metabolic rate and protein synthesis, and in children, growth and development. Calcitonin plays a role in calcium homeostasis. Secretion of the two thyroid hormones is regulated by thyroid-stimulating hormone (TSH), which is secreted from the anterior pituitary gland. TSH is regulated by thyrotropin-releasing hormone (TRH), which is produced by the hypothalamus.
Hypothyroidism is a disorder of the endocrine system in which the thyroid gland does not produce enough thyroid hormone. It can cause a number of symptoms, such as poor ability to tolerate cold, a feeling of tiredness, constipation, slow heart rate, depression, and weight gain. Occasionally there may be swelling of the front part of the neck due to goiter. Untreated cases of hypothyroidism during pregnancy can lead to delays in growth and intellectual development in the baby or congenital iodine deficiency syndrome.
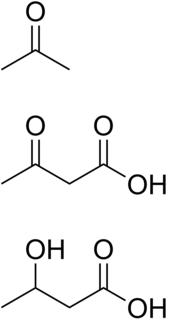
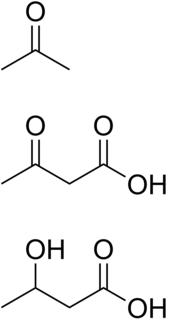
Ketosis is a metabolic state characterized by elevated levels of ketone bodies in the blood or urine. Physiologic ketosis is a normal response to low glucose availability, such as low-carbohydrate diets or fasting, that provides an additional energy source for the brain in the form of ketones. In physiologic ketosis, ketones in the blood are elevated above baseline levels, but the body's acid–base homeostasis is maintained. This contrasts with ketoacidosis, an uncontrolled production of ketones that occurs in pathologic states and causes a metabolic acidosis, which is a medical emergency. Ketoacidosis is most commonly the result of complete insulin deficiency in type 1 diabetes or late-stage type 2 diabetes. Ketone levels can be measured in blood, urine or breath and are generally between 0.5 and 3.0 millimolar (mM) in physiologic ketosis, while ketoacidosis may cause blood concentrations greater than 10 mM.
Appetite is the desire to eat food, sometimes due to hunger. Appealing foods can stimulate appetite even when hunger is absent, although appetite can be greatly reduced by satiety. Appetite exists in all higher life-forms, and serves to regulate adequate energy intake to maintain metabolic needs. It is regulated by a close interplay between the digestive tract, adipose tissue and the brain. Appetite has a relationship with every individual's behavior. Appetitive behaviour also known as approach behaviour, and consummatory behaviour, are the only processes that involve energy intake, whereas all other behaviours affect the release of energy. When stressed, appetite levels may increase and result in an increase of food intake. Decreased desire to eat is termed anorexia, while polyphagia is increased eating. Dysregulation of appetite contributes to anorexia nervosa, bulimia nervosa, cachexia, overeating, and binge eating disorder.

Exercise physiology is the physiology of physical exercise. It is one of the allied health professions that involves the study of the acute responses and chronic adaptations to exercise. Exercise Physiologists are the highest qualified exercise professionals and utilise education, lifestyle intervention and specific forms of exercise to rehabilitate and manage acute and chronic injuries and conditions.
Basal metabolic rate (BMR) is the rate of energy expenditure per unit time by endothermic animals at rest. It is reported in energy units per unit time ranging from watt (joule/second) to ml O2/min or joule per hour per kg body mass J/(h·kg). Proper measurement requires a strict set of criteria to be met. These criteria include being in a physically and psychologically undisturbed state and being in a thermally neutral environment while in the post-absorptive state (i.e., not actively digesting food). In bradymetabolic animals, such as fish and reptiles, the equivalent term standard metabolic rate (SMR) applies. It follows the same criteria as BMR, but requires the documentation of the temperature at which the metabolic rate was measured. This makes BMR a variant of standard metabolic rate measurement that excludes the temperature data, a practice that has led to problems in defining "standard" rates of metabolism for many mammals.

Hyperplasia, or hypergenesis, is an enlargement of an organ or tissue caused by an increase in the amount of organic tissue that results from cell proliferation. It may lead to the gross enlargement of an organ, and the term is sometimes confused with benign neoplasia or benign tumor.
Hypermetabolism is defined as an elevated resting energy expenditure (REE) > 110% of predicted REE. Hypermetabolism is accompanied by a variety of internal and external symptoms, most notably extreme weight loss, and can also be a symptom in itself. This state of increased metabolic activity can signal underlying issues, especially hyperthyroidism. Patients with Fatal familial insomnia, an extremely rare and strictly hereditary disorder, also presents with hypermetabolism; however, this universally fatal disorder is exceedingly rare, with only a few known cases worldwide. The drastic impact of the hypermetabolic state on patient nutritional requirements is often understated or overlooked as well.

Thyroid disease is a medical condition that affects the function of the thyroid gland. The thyroid gland is located at the front of the neck and produces thyroid hormones that travel through the blood to help regulate many other organs, meaning that it is an endocrine organ. These hormones normally act in the body to regulate energy use, infant development, and childhood development.
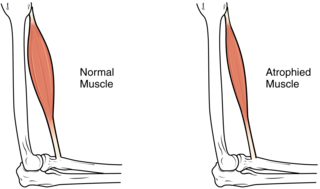
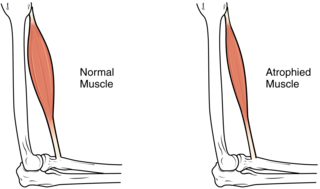
Muscle atrophy is the loss of skeletal muscle mass. It can be caused by immobility, aging, malnutrition, medications, or a wide range of injuries or diseases that impact the musculoskeletal or nervous system. Muscle atrophy leads to muscle weakness and causes disability.
Euthyroid sick syndrome (ESS) is a state of adaptation or dysregulation of thyrotropic feedback control wherein the levels of T3 and/or T4 are abnormal, but the thyroid gland does not appear to be dysfunctional. This condition may result from allostatic responses of hypothalamus-pituitary-thyroid feedback control, dyshomeostatic disorders, drug interferences, and impaired assay characteristics in critical illness.
Chronic stress is the response to emotional pressure suffered for a prolonged period of time in which an individual perceives they have little or no control. It involves an endocrine system response in which corticosteroids are released. While the immediate effects of stress hormones are beneficial in a particular short-term situation, long-term exposure to stress creates a high level of these hormones. This may lead to high blood pressure, damage to muscle tissue, inhibition of growth, and damage to mental health.
In cell biology and pathophysiology, cellular adaptation refers to changes made by a cell in response to adverse or varying environmental changes. The adaptation may be physiologic (normal) or pathologic (abnormal). Four types of morphological adaptations include atrophy, hypertrophy, hyperplasia, and metaplasia.
Functional hypothalamic amenorrhea (FHA) is a form of amenorrhea and chronic anovulation and is one of the most common types of secondary amenorrhea. It is classified as hypogonadotropic hypogonadism. It was previously known as "juvenile hypothalamosis syndrome," prior to the discovery that sexually mature females are equally affected. FHA has multiple risk factors, with links to stress-related, weight-related, and exercise-related factors. FHA is caused by stress-induced suppression of the hypothalamic-pituitary-ovarian (HPO) axis, which results in inhibition of gonadotropin-releasing hormone (GnRH) secretion, and gonadotropins, follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Severe and potentially prolonged hypoestrogenism is perhaps the most dangerous hormonal pathology associated with the disease, because consequences of this disturbance can influence bone health, cardiovascular health, mental health, and metabolic functioning in both the short and long-term. Because many of the symptoms overlap with those of organic hypothalamic, pituitary, or gonadal disease and therefore must be ruled out, FHA is a diagnosis of exclusion; "functional" is used to indicate a behavioral cause, in which no anatomical or organic disease is identified, and is reversible with correction of the underlying cause. Diagnostic workup includes a detailed history and physical, laboratory studies, such as a pregnancy test, and serum levels of FSH and LH, prolactin, and thyroid-stimulating hormone (TSH), and imaging. Additional tests may be indicated in order to distinguish FHA from organic hypothalamic or pituitary disorders. Patients present with a broad range of symptoms related to severe hypoestrogenism as well as hypercortisolemia, low serum insulin levels, low serum insulin-like growth factor 1 (IGF-1), and low total triiodothyronine (T3). Treatment is primarily managing the primary cause of the FHA with behavioral modifications. While hormonal-based therapies are potential treatment to restore menses, weight gain and behavioral modifications can have an even more potent impact on reversing neuroendocrine abnormalities, preventing further bone loss, and re-establishing menses, making this the recommended line of treatment. If this fails to work, secondary treatment is aimed at treating the effects of hypoestrogenism, hypercortisolism, and hypothyroidism.
An endocrine bone disease is a bone disease associated with a disorder of the endocrine system. An example is osteitis fibrosa cystica.
Hypothalamic disease is a disorder presenting primarily in the hypothalamus, which may be caused by damage resulting from malnutrition, including anorexia and bulimia eating disorders, genetic disorders, radiation, surgery, head trauma, lesion, tumour or other physical injury to the hypothalamus. The hypothalamus is the control center for several endocrine functions. Endocrine systems controlled by the hypothalamus are regulated by antidiuretic hormone (ADH), corticotropin-releasing hormone, gonadotropin-releasing hormone, growth hormone-releasing hormone, oxytocin, all of which are secreted by the hypothalamus. Damage to the hypothalamus may impact any of these hormones and the related endocrine systems. Many of these hypothalamic hormones act on the pituitary gland. Hypothalamic disease therefore affects the functioning of the pituitary and the target organs controlled by the pituitary, including the adrenal glands, ovaries and testes, and the thyroid gland.
Iodine is an essential trace element in biological systems. It has the distinction of being the heaviest element commonly needed by living organisms as well as the second-heaviest known to be used by any form of life. It is a component of biochemical pathways in organisms from all biological kingdoms, suggesting its fundamental significance throughout the evolutionary history of life.

Weight management includes the techniques and physiological processes that contribute to a person's ability to attain and maintain a certain weight. Most weight management techniques encompass long-term lifestyle strategies that promote healthy eating and daily physical activity. Moreover, weight management involves developing meaningful ways to track weight over time and to identify ideal body weights for different individuals.

Thyrotoxic periodic paralysis (TPP) is a condition featuring attacks of muscle weakness in the presence of hyperthyroidism. Hypokalemia is usually present during attacks. The condition may be life-threatening if weakness of the breathing muscles leads to respiratory failure, or if the low potassium levels lead to cardiac arrhythmias. If untreated, it is typically recurrent in nature.