Related Research Articles

Sleep apnea, British English sleep apnoea or sleep apnœa, is a sleep-related breathing disorder in which repetitive pauses in breathing, periods of shallow breathing, or collapse of the upper airway during sleep results in poor ventilation and sleep disruption. Each pause in breathing can last for a few seconds to a few minutes and occurs many times a night. A choking or snorting sound may occur as breathing resumes. Common symptoms include daytime sleepiness, snoring, and non restorative sleep despite adequate sleep time. Because the disorder disrupts normal sleep, those affected may experience sleepiness or feel tired during the day. It is often a chronic condition.

The sleep cycle is an oscillation between the slow-wave and REM (paradoxical) phases of sleep. It is sometimes called the ultradian sleep cycle, sleep–dream cycle, or REM-NREM cycle, to distinguish it from the circadian alternation between sleep and wakefulness. In humans, this cycle takes 70 to 110 minutes. Within the sleep of adults and infants there are cyclic fluctuations between quiet and active sleep. These fluctuations may persist during wakefulness as rest-activity cycles but are less easily discerned.

Delta waves are high amplitude neural oscillations with a frequency between 0.5 and 4 hertz. Delta waves, like other brain waves, can be recorded with electroencephalography (EEG) and are usually associated with the deep stage 3 of NREM sleep, also known as slow-wave sleep (SWS), and aid in characterizing the depth of sleep. Suppression of delta waves leads to inability of body rejuvenation, brain revitalization and poor sleep.
Non-rapid eye movement sleep (NREM), also known as quiescent sleep, is, collectively, sleep stages 1–3, previously known as stages 1–4. Rapid eye movement sleep (REM) is not included. There are distinct electroencephalographic and other characteristics seen in each stage. Unlike REM sleep, there is usually little or no eye movement during these stages. Dreaming occurs during both sleep states, and muscles are not paralyzed as in REM sleep. People who do not go through the sleeping stages properly get stuck in NREM sleep, and because muscles are not paralyzed a person may be able to sleepwalk. According to studies, the mental activity that takes place during NREM sleep is believed to be thought-like, whereas REM sleep includes hallucinatory and bizarre content. NREM sleep is characteristic of dreamer-initiated friendliness, compared to REM sleep where it is more aggressive, implying that NREM is in charge of simulating friendly interactions. The mental activity that occurs in NREM and REM sleep is a result of two different mind generators, which also explains the difference in mental activity. In addition, there is a parasympathetic dominance during NREM. The reported differences between the REM and NREM activity are believed to arise from differences in the memory stages that occur during the two types of sleep.
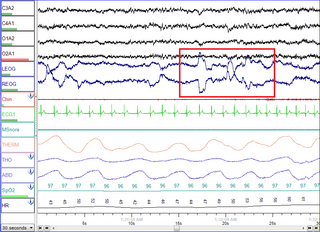
Polysomnography (PSG) is a multi-parameter type of sleep study and a diagnostic tool in sleep medicine. The test result is called a polysomnogram, also abbreviated PSG. The name is derived from Greek and Latin roots: the Greek πολύς, the Latin somnus ("sleep"), and the Greek γράφειν.
Sleep spindles are bursts of neural oscillatory activity that are generated by interplay of the thalamic reticular nucleus (TRN) and other thalamic nuclei during stage 2 NREM sleep in a frequency range of ~11 to 16 Hz with a duration of 0.5 seconds or greater. After generation as an interaction of the TRN neurons and thalamocortical cells, spindles are sustained and relayed to the cortex by thalamo-thalamic and thalamo-cortical feedback loops regulated by both GABAergic and NMDA-receptor mediated glutamatergic neurotransmission. Sleep spindles have been reported for all tested mammalian species. Considering animals in which sleep-spindles were studied extensively, they appear to have a conserved main frequency of roughly 9–16 Hz. Only in humans, rats and dogs is a difference in the intrinsic frequency of frontal and posterior spindles confirmed, however.

Lennox–Gastaut syndrome (LGS) is a complex, rare, and severe childhood-onset epilepsy syndrome. It is characterized by multiple and concurrent seizure types including tonic seizure, cognitive dysfunction, and slow spike waves on electroencephalogram (EEG), which are very abnormal. Typically, it presents in children aged 3–5 years and most of the time persists into adulthood with slight changes in the electroclinical phenotype. It has been associated with perinatal injuries, congenital infections, brain malformations, brain tumors, genetic disorders such as tuberous sclerosis and numerous gene mutations. Sometimes LGS is observed after infantile epileptic spasm syndrome. The prognosis for LGS is marked by a 5% mortality in childhood and persistent seizures into adulthood.

Slow-wave sleep (SWS), often referred to as deep sleep, is the third stage of non-rapid eye movement sleep (NREM), where electroencephalography activity is characterised by slow delta waves.

Hypsarrhythmia is very chaotic and disorganized brain electrical activity with no recognizable pattern, whereas a normal brain electrical activity shows clear separation between each signal and visible pattern. It is an abnormal interictal pattern, consisting of high amplitude and irregular waves and spikes in a background of chaotic and disorganized activity seen on electroencephalogram (EEG), and frequently encountered in infants diagnosed with infantile spasms, although it can be found in other conditions such as tuberous sclerosis.
Parasomnias are a category of sleep disorders that involve abnormal movements, behaviors, emotions, perceptions, and dreams that occur while falling asleep, sleeping, between sleep stages, or during arousal from sleep. Parasomnias are dissociated sleep states which are partial arousals during the transitions between wakefulness, NREM sleep, and REM sleep, and their combinations.
Rhythmic movement disorder (RMD) is a neurological disorder characterized by repetitive movements of large muscle groups immediately before and during sleep often involving the head and neck. It was independently described first in 1905 by Zappert as jactatio capitis nocturna and by Cruchet as rhythmie du sommeil. The majority of RMD episodes occur during NREM sleep, although REM movements have been reported. RMD is often associated with other psychiatric conditions or mental disabilities. The disorder often leads to bodily injury from unwanted movements. Because of these incessant muscle contractions, patients' sleep patterns are often disrupted. It differs from restless legs syndrome in that RMD involves involuntary muscle contractions before and during sleep while restless legs syndrome is the urge to move before sleep. RMD occurs in both males and females, often during early childhood with symptoms diminishing with age. Many affected individuals also have other sleep related disorders, like sleep apnea. The disorder can be differentially diagnosed into small subcategories, including sleep related bruxism, thumb sucking, hypnagogic foot tremor, and rhythmic sucking, to name a few. In order to be considered pathological, the ICSD-II requires that in the sleep-related rhythmic movements should “markedly interfere with normal sleep, cause significant impairment in daytime function, or result in self-inflicted bodily injury that requires medical treatment ”.
Hypopnea is overly shallow breathing or an abnormally low respiratory rate. Hypopnea is typically defined by a decreased amount of air movement into the lungs and can cause hypoxemia It commonly is due to partial obstruction of the upper airway, but can also have neurological origins in central sleep apnea.

Catathrenia or nocturnal groaning is a sleep-related breathing disorder, consisting of end-inspiratory apnea and expiratory groaning during sleep. It describes a rare condition characterized by monotonous, irregular groans while sleeping. Catathrenia begins with a deep inspiration. The person with catathrenia holds his or her breath against a closed glottis, similar to the Valsalva maneuver. Expiration can be slow and accompanied by sound caused by vibration of the vocal cords or a simple rapid exhalation. Despite a slower breathing rate, no oxygen desaturation usually occurs. The moaning sound is usually not noticed by the person producing the sound, but it can be extremely disturbing to sleep partners. It appears more often during expiration REM sleep than in NREM sleep.

The Safe to Sleep campaign, formerly known as the Back to Sleep campaign, is an initiative backed by the US National Institute of Child Health and Human Development (NICHD) at the US National Institutes of Health to encourage parents to have their infants sleep on their backs to reduce the risk of sudden infant death syndrome, or SIDS. The target age group of the campaign is 0–1 years of age, because this is when babies are at the greatest risk of experiencing SIDS. Since "Safe to Sleep" was launched in 1994, the incidence of SIDS has declined by more than 50%. However, there has been a rise in infant sleep-related suffocation events. Consequently, the campaign has broadened its goal to focus on safe sleep conditions and further preventative measures.

Sleep in animals refers to a behavioral and physiological state characterized by altered consciousness, reduced responsiveness to external stimuli, and homeostatic regulation observed in various animals. Sleep has been observed in mammals, birds, reptiles, amphibians, and some fish, and, in some form, in insects and even in simpler animals such as nematodes. The internal circadian clock promotes sleep at night for diurnal organisms and in the day for nocturnal organisms. Sleep patterns vary widely among species. It appears to be a requirement for all mammals and most other animals.
Ponto-geniculo-occipital waves or PGO waves are distinctive wave forms of propagating activity between three key brain regions: the pons, lateral geniculate nucleus, and occipital lobe; specifically, they are phasic field potentials. These waves can be recorded from any of these three structures during and immediately before REM sleep. The waves begin as electrical pulses from the pons, then move to the lateral geniculate nucleus residing in the thalamus, and end in the primary visual cortex of the occipital lobe. The appearances of these waves are most prominent in the period right before REM sleep, albeit they have been recorded during wakefulness as well. They are theorized to be intricately involved with eye movement of both wake and sleep cycles in many different animals.

A hypnogram is a form of polysomnography; it is a graph that represents the stages of sleep as a function of time. It was developed as an easy way to present the recordings of the brain wave activity from an electroencephalogram (EEG) during a period of sleep. It allows the different stages of sleep: rapid eye movement sleep (REM) and non-rapid eye movement sleep (NREM) to be identified during the sleep cycle. NREM sleep can be further classified into NREM stage 1, 2 and 3. The previously considered 4th stage of NREM sleep has been included within stage 3; this stage is also called slow wave sleep (SWS) and is the deepest stage of sleep.

The neuroscience of sleep is the study of the neuroscientific and physiological basis of the nature of sleep and its functions. Traditionally, sleep has been studied as part of psychology and medicine. The study of sleep from a neuroscience perspective grew to prominence with advances in technology and the proliferation of neuroscience research from the second half of the twentieth century.
A confusional arousal is medical condition where a person awakened from sleep shows mental confusion for at least several minutes. Complete or partial amnesia of the episodes may be present.

Behavioral sleep medicine (BSM) is a field within sleep medicine that encompasses scientific inquiry and clinical treatment of sleep-related disorders, with a focus on the psychological, physiological, behavioral, cognitive, social, and cultural factors that affect sleep, as well as the impact of sleep on those factors. The clinical practice of BSM is an evidence-based behavioral health discipline that uses primarily non-pharmacological treatments. BSM interventions are typically problem-focused and oriented towards specific sleep complaints, but can be integrated with other medical or mental health treatments. The primary techniques used in BSM interventions involve education and systematic changes to the behaviors, thoughts, and environmental factors that initiate and maintain sleep-related difficulties.
References
- ↑ Terzano, M. G.; Mancia, D.; Salati, M. R.; Costani, G.; Decembrino, A.; Parrino, L. (1985). "The cyclic alternating pattern as a physiologic component of normal NREM sleep". Sleep. 8 (2): 137–145. doi: 10.1093/sleep/8.2.137 . ISSN 0161-8105. PMID 4012156.
- ↑ Kryger (2017). Principles and Practice of Sleep Medicine. Elsevier. p. 1576. ISBN 9780323242882.
- ↑ Parrino, Liborio; Grassi, Andrea; Milioli, Giulia (November 2014). "Cyclic alternating pattern in polysomnography: what is it and what does it mean?". Current Opinion in Pulmonary Medicine. 20 (6): 533–541. doi: 10.1097/MCP.0000000000000100 . ISSN 1531-6971. PMID 25188718.
- ↑ Parrino, Liborio; Ferri, Raffaele; Bruni, Oliviero; Terzano, Mario G. (February 2012). "Cyclic alternating pattern (CAP): the marker of sleep instability". Sleep Medicine Reviews. 16 (1): 27–45. doi:10.1016/j.smrv.2011.02.003. ISSN 1532-2955. PMID 21616693.
- ↑ Eisensehr, I.; Parrino, L.; Noachtar, S.; Smerieri, A.; Terzano, M.G. (2001-09-01). "Sleep in Lennox–Gastaut syndrome: the role oft the cyclic alternating pattern (CAP) in the gate control of clinical seizures and generalized polyspikes". Epilepsy Research. 46 (3): 241–250. doi:10.1016/S0920-1211(01)00280-7. ISSN 0920-1211. PMID 11518625.
- 1 2 Kryger (2017). Principles and Practice of Sleep Medicine. Elsevier. pp. 1586–1587. ISBN 9780323242882.
- ↑ "Cyclic alternating pattern". www.medlink.com. Retrieved 2018-11-08.
- ↑ "A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. Allan Rechtschaffen and Anthony Kales, editors. - NLM Catalog - NCBI". www.ncbi.nlm.nih.gov. Retrieved 2018-11-08.
- ↑ Boselli, M.; Parrino, L.; Smerieri, A.; Terzano, M. G. (1998-06-15). "Effect of age on EEG arousals in normal sleep". Sleep. 21 (4): 351–357. ISSN 0161-8105. PMID 9646379.