Related Research Articles

In aphasia, a person may be unable to comprehend or unable to formulate language because of damage to specific brain regions. The major causes are stroke and head trauma; prevalence is hard to determine, but aphasia due to stroke is estimated to be 0.1–0.4% in the Global North. Aphasia can also be the result of brain tumors, epilepsy, autoimmune neurological diseases, brain infections, or neurodegenerative diseases.
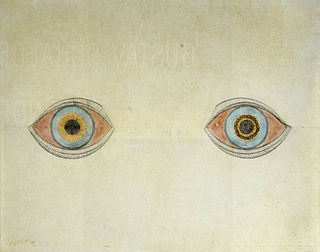
A hallucination is a perception in the absence of an external stimulus that has the compelling sense of reality. They are distinguishable from several related phenomena, such as dreaming, which does not involve wakefulness; pseudohallucination, which does not mimic real perception, and is accurately perceived as unreal; illusion, which involves distorted or misinterpreted real perception; and mental imagery, which does not mimic real perception, and is under voluntary control. Hallucinations also differ from "delusional perceptions", in which a correctly sensed and interpreted stimulus is given some additional significance.

Apraxia is a motor disorder caused by damage to the brain, which causes difficulty with motor planning to perform tasks or movements. The nature of the damage determines the disorder's severity, and the absence of sensory loss or paralysis helps to explain the level of difficulty. Children may be born with apraxia; its cause is unknown, and symptoms are usually noticed in the early stages of development. Apraxia occurring later in life, known as acquired apraxia, is typically caused by traumatic brain injury, stroke, dementia, Alzheimer's disease, brain tumor, or other neurodegenerative disorders. The multiple types of apraxia are categorized by the specific ability and/or body part affected.

Brain injury (BI) is the destruction or degeneration of brain cells. Brain injuries occur due to a wide range of internal and external factors. In general, brain damage refers to significant, undiscriminating trauma-induced damage.

The parietal lobe is one of the four major lobes of the cerebral cortex in the brain of mammals. The parietal lobe is positioned above the temporal lobe and behind the frontal lobe and central sulcus.

The temporal lobe is one of the four major lobes of the cerebral cortex in the brain of mammals. The temporal lobe is located beneath the lateral fissure on both cerebral hemispheres of the mammalian brain.
Anosognosia is a condition in which a person with a disability is cognitively unaware of having it due to an underlying physical condition. Anosognosia results from physiological damage to brain structures, typically to the parietal lobe or a diffuse lesion on the fronto-temporal-parietal area in the right hemisphere, and is thus a neuropsychiatric disorder. A deficit of self-awareness, the term was first coined by the neurologist Joseph Babinski in 1914, in order to describe the unawareness of hemiplegia.
Cerebral atrophy is a common feature of many of the diseases that affect the brain. Atrophy of any tissue means a decrement in the size of the cell, which can be due to progressive loss of cytoplasmic proteins. In brain tissue, atrophy describes a loss of neurons and the connections between them. Brain atrophy can be classified into two main categories: generalized and focal atrophy. Generalized atrophy occurs across the entire brain whereas focal atrophy affects cells in a specific location. If the cerebral hemispheres are affected, conscious thought and voluntary processes may be impaired.

An aura is a perceptual disturbance experienced by some with epilepsy or migraine. An epileptic aura is actually a minor seizure.

Monoplegia is paralysis of a single limb, usually an arm. Common symptoms associated with monoplegic patients are weakness, numbness, and pain in the affected limb. Monoplegia is a type of paralysis that falls under hemiplegia. While hemiplegia is paralysis of half of the body, monoplegia is localized to a single limb or to a specific region of the body. Monoplegia of the upper limb is sometimes referred to as brachial monoplegia, and that of the lower limb is called crural monoplegia. Monoplegia in the lower extremities is not as common of an occurrence as in the upper extremities. Monoparesis is a similar, but less severe, condition because one limb is very weak, not paralyzed. For more information, see paresis.
Focal seizures are seizures that affect initially only one hemisphere of the brain. The brain is divided into two hemispheres, each consisting of four lobes – the frontal, temporal, parietal and occipital lobes. A focal seizure is generated in and affects just one part of the brain – a whole hemisphere or part of a lobe. Symptoms will vary according to where the seizure occurs. When seizures occur in the frontal lobe, the patient may experience a wave-like sensation in the head. When seizures occur in the temporal lobe, a feeling of déjà vu may be experienced. When seizures are localized to the parietal lobe, a numbness or tingling may occur. With seizures occurring in the occipital lobe, visual disturbances or hallucinations have been reported.
This glossary covers terms found in the psychiatric literature; the word origins are primarily Greek, but there are also Latin, French, German, and English terms. Many of these terms refer to expressions dating from the early days of psychiatry in Europe.
In the field of neurology, seizure types are categories of seizures defined by seizure behavior, symptoms, and diagnostic tests. The International League Against Epilepsy (ILAE) 2017 classification of seizures is the internationally recognized standard for identifying seizure types. The ILAE 2017 classification of seizures is a revision of the prior ILAE 1981 classification of seizures. Distinguishing between seizure types is important since different types of seizures may have different causes, outcomes, and treatments.

Foix–Chavany–Marie syndrome (FCMS), also known as bilateral opercular syndrome, is a neuropathological disorder characterized by paralysis of the facial, tongue, pharynx, and masticatory muscles of the mouth that aid in chewing. The disorder is primarily caused by thrombotic and embolic strokes, which cause a deficiency of oxygen in the brain. As a result, bilateral lesions may form in the junctions between the frontal lobe and temporal lobe, the parietal lobe and cortical lobe, or the subcortical region of the brain. FCMS may also arise from defects existing at birth that may be inherited or nonhereditary. Symptoms of FCMS can be present in a person of any age and it is diagnosed using automatic-voluntary dissociation assessment, psycholinguistic testing, neuropsychological testing, and brain scanning. Treatment for FCMS depends on the onset, as well as on the severity of symptoms, and it involves a multidisciplinary approach.
Todd's paresis is focal weakness in a part or all of the body after a seizure. This weakness typically affects the limbs and is localized to either the left or right side of the body. It usually subsides completely within 48 hours. Todd's paresis may also affect speech, eye position (gaze), or vision.
Apperceptive agnosia is a neurological disorder characterized by failures in recognition due to a failure of perception. In contrast, associative agnosia is a type of agnosia where perception occurs but recognition still does not occur. When referring to apperceptive agnosia, visual and object agnosia are most commonly discussed; this occurs because apperceptive agnosia is most likely to present visual impairments. However, in addition to visual apperceptive agnosia there are also cases of apperceptive agnosia in other sensory areas.
Transient epileptic amnesia (TEA) is a rare but probably underdiagnosed neurological condition which manifests as relatively brief and generally recurring episodes of amnesia caused by underlying temporal lobe epilepsy. Though descriptions of the condition are based on fewer than 100 cases published in the medical literature, and the largest single study to date included 50 people with TEA, TEA offers considerable theoretical significance as competing theories of human memory attempt to reconcile its implications.
The neuroanatomy of memory encompasses a wide variety of anatomical structures in the brain.
Charcot–Wilbrand syndrome (CWS) is dream loss following focal brain damage specifically characterised by visual agnosia and loss of ability to mentally recall or "revisualize" images. The name of this condition dates back to the case study work of Jean-Martin Charcot and Hermann Wilbrand, and was first described by Otto Potzl as "mind blindness with disturbance of optic imagination". MacDonald Critchley, former president of the World Federation of Neurology, more recently summarized CWS as "a patient loses the power to conjure up visual images or memories, and furthermore, ceases to dream during his sleeping hours". This condition is quite rare and affects only a handful of brain damage patients. Further study could help illuminate the neurological pathway for dream formation.
A somatosensory disorder is an impairment of the somatosensory system.
References
- ↑ Thiruppathy, S. P.; Muthukumar, N. (2004). "Mild head injury: Revisited". Acta Neurochirurgica. 146 (10): 1075–82, discussion 1082-3. doi:10.1007/s00701-004-0335-z. PMID 15744844. S2CID 13150034.
- ↑ Thal, G. D.; Szabo, M. D.; Lopez-Bresnahan, M.; Crosby, G. (1996). "Exacerbation or unmasking of focal neurologic deficits by sedatives". Anesthesiology. 85 (1): 21–5, discussion 29A-30A. doi: 10.1097/00000542-199607000-00004 . PMID 8694368. S2CID 8984607.
- 1 2 3 4 Fountoulakis, KN; Panagiotidis, P; Kimiskidis, V; Nimatoudis, I; Gonda, X (February 2019). "Neurological soft signs in familial and sporadic schizophrenia". Psychiatry Research. 272: 222–229. doi:10.1016/j.psychres.2018.12.105. PMID 30590276. S2CID 56476015.
- ↑ Ferri, Fred F. (2019). Ferri's clinical advisor 2019 : 5 books in 1. pp. 1225–1226. ISBN 9780323530422.
Essentials of Kumar and Clark's Clinical Medicine, 5th Edition. Saunders Elsevier, UK. 2012. page 725