Medicare is an unofficial designation used to refer to the publicly funded single-payer healthcare system of Canada. Canada's health care system consists of 13 provincial and territorial health insurance plans, which provide universal healthcare coverage to Canadian citizens, permanent residents, and depending on the province or territory, certain temporary residents. The systems are individually administered on a provincial or territorial basis, within guidelines set by the federal government. The formal terminology for the insurance system is provided by the Canada Health Act and the health insurance legislation of the individual provinces and territories.
A health system, health care system or healthcare system is an organization of people, institutions, and resources that delivers health care services to meet the health needs of target populations.
Health insurance or medical insurance is a type of insurance that covers the whole or a part of the risk of a person incurring medical expenses. As with other types of insurance, risk is shared among many individuals. By estimating the overall risk of health risk and health system expenses over the risk pool, an insurer can develop a routine finance structure, such as a monthly premium or payroll tax, to provide the money to pay for the health care benefits specified in the insurance agreement. The benefit is administered by a central organization, such as a government agency, private business, or not-for-profit entity.

Healthcare in Canada is delivered through the provincial and territorial systems of publicly funded health care, informally called Medicare. It is guided by the provisions of the Canada Health Act of 1984, and is universal. The 2002 Royal Commission, known as the Romanow Report, revealed that Canadians consider universal access to publicly funded health services as a "fundamental value that ensures national health care insurance for everyone wherever they live in the country."

Two-tier healthcare is a situation in which a basic government-provided healthcare system provides basic care, and a secondary tier of care exists for those who can pay for additional, better quality or faster access. Most countries have both publicly and privately funded healthcare, but the degree to which it creates a quality differential depends on the way the two systems are managed, funded, and regulated.
Health care in Ireland is delivered through public and private healthcare. The public health care system is governed by the Health Act 2004, which established a new body to be responsible for providing health and personal social services to everyone living in Ireland – the Health Service Executive. The new national health service came into being officially on 1 January 2005; however the new structures are currently in the process of being established as the reform programme continues. In addition to the public-sector, there is also a large private healthcare market.

The health care system in Japan provides different types of services, including screening examinations, prenatal care and infectious disease control, with the patient accepting responsibility for 30% of these costs while the government pays the remaining 70%. Payment for personal medical services is offered by a universal health care insurance system that provides relative equality of access, with fees set by a government committee. All residents of Japan are required by the law to have health insurance coverage. People without insurance from employers can participate in a national health insurance program, administered by local governments. Patients are free to select physicians or facilities of their choice and cannot be denied coverage. Hospitals, by law, must be run as non-profits and be managed by physicians.

Healthcare in the United Kingdom is a devolved matter, with England, Northern Ireland, Scotland and Wales each having their own systems of publicly funded healthcare, funded by and accountable to separate governments and parliaments, together with smaller private sector and voluntary provision. As a result of each country having different policies and priorities, a variety of differences have developed between these systems since devolution.

Healthcare in South Korea is universal, although a significant portion of healthcare is privately funded. South Korea's healthcare system is based on the National Health Insurance Service, a public health insurance program run by the Ministry of Health and Welfare to which South Koreans of sufficient income must pay contributions in order to insure themselves and their dependants, and the Medical Aid Program, a social welfare program run by the central government and local governments to insure those unable to pay National Health Insurance contributions. In 2015, South Korea ranked first in the OECD for healthcare access. Satisfaction of healthcare has been consistently among the highest in the world – South Korea was rated as the second most efficient healthcare system by Bloomberg. Health insurance in South Korea is single-payer system. The introduction of health insurance resulted in a significant surge in the utilization of healthcare services. Healthcare providers are overburdened by government taking advantage of them.
Healthcare in Finland consists of a highly decentralized three-level publicly funded healthcare system and a much smaller private sector. Although the Ministry of Social Affairs and Health has the highest decision-making authority, specific healthcare precincts are responsible for providing healthcare to their residents as of 2023.
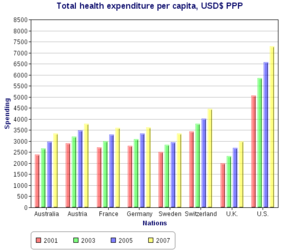
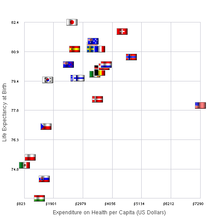
The French health care system is one of universal health care largely financed by government national health insurance. In its 2000 assessment of world health care systems, the World Health Organization found that France provided the "best overall health care" in the world. In 2017, France spent 11.3% of GDP on health care, or US$5,370 per capita, a figure higher than the average spent by rich countries, though similar to Germany (10.6%) and Canada (10%), but much less than in the US. Approximately 77% of health expenditures are covered by government funded agencies.

Spain operates a universal health care system. According to the Organisation for Economic Co-operation and Development, total health spending accounted for 9.4% of GDP in Spain in 2011, slightly above the OECD average of 9.3%. Spain's healthcare system ranks 19th in Europe according to the 2018 Euro health consumer index. As of 2016, Spain is ranked 1st in the world in organ transplants.

Italy's healthcare system is consistently ranked among the best in the world. The Italian healthcare system employs a Beveridge model, and operates on the assumption that health care is a human right that should be provided to everyone regardless of their ability to pay. Life expectancy is the 4th highest among OECD countries and the world's 8th highest according to the WHO. Healthcare spending accounted for 9.7% of GDP in 2020.

Healthcare in Denmark is largely provided by the local governments of the five regions, with coordination and regulation by central government, while nursing homes, home care, and school health services are the responsibility of the 98 municipalities. Some specialised hospital services are managed centrally.

Healthcare in Slovenia is organised primarily through the Health Insurance Institute of Slovenia. In 2015, healthcare expenditures accounted for 8.10% of GDP. The Slovenian healthcare system was ranked 15th in the Euro health consumer index 2015. The country ranked second in the 2012 Euro Hepatitis Index.

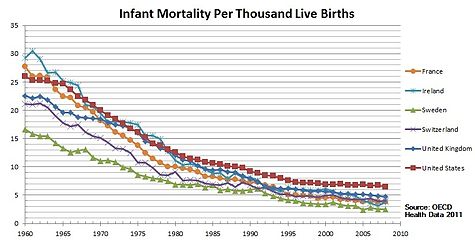
Healthcare in the United States is largely provided by private sector healthcare facilities, and paid for by a combination of public programs, private insurance, and out-of-pocket payments. The U.S. is the only developed country without a system of universal healthcare, and a significant proportion of its population lacks health insurance. The United States spends more on healthcare than any other country, both in absolute terms and as a percentage of GDP; however, this expenditure does not necessarily translate into better overall health outcomes compared to other developed nations. Coverage varies widely across the population, with certain groups, such as the elderly and low-income individuals, receiving more comprehensive care through government programs such as Medicaid and Medicare.
In Norway, municipalities are in charge of providing basic healthcare. Since the money given to municipalities is not set aside for any particular purpose, each municipality is free to determine its own health budget. Municipalities coordinate primary healthcare services through agreements with independent physicians. In Norway, private healthcare providers are not compensated unless they have a contract with the public health service.

Healthcare in Belgium is composed of three parts. Firstly there is a primarily publicly funded healthcare and social security service run by the federal government, which organises and regulates healthcare; independent private/public practitioners, university/semi-private hospitals and care institutions. There are a few private hospitals. Secondly is the insurance coverage provided for patients. Finally, industry coverage; which covers the production and distribution of healthcare products for research and development. The primary aspect of this research is done in universities and hospitals.
Examples of health care systems of the world, sorted by continent, are as follows.