Post-traumatic stress disorder (PTSD) is a mental and behavioral disorder that can develop because of exposure to a traumatic event, such as sexual assault, warfare, traffic collisions, child abuse, domestic violence, or other threats on a person's life. Symptoms may include disturbing thoughts, feelings, or dreams related to the events, mental or physical distress to trauma-related cues, attempts to avoid trauma-related cues, alterations in the way a person thinks and feels, and an increase in the fight-or-flight response. These symptoms last for more than a month after the event. Young children are less likely to show distress but instead may express their memories through play. A person with PTSD is at a higher risk of suicide and intentional self-harm.
The Veterans Health Administration (VHA) is the component of the United States Department of Veterans Affairs (VA) led by the Under Secretary of Veterans Affairs for Health that implements the healthcare program of the VA through a nationalized healthcare service in the United States, providing healthcare and healthcare-adjacent services to Veterans through the administration and operation of 146 VA Medical Centers (VAMC) with integrated outpatient clinics, 772 Community Based Outpatient Clinics (CBOC), and 134 VA Community Living Centers Programs. It is the largest division in the Department, and second largest in the entire federal government, employing over 350,000 employees. All VA hospitals, clinics and medical centers are owned by and operated by the Department of Veterans Affairs as opposed to private companies, and all of the staff employed in VA hospitals are government employees. Because of this, Veterans that qualify for VHA healthcare do not pay premiums or deductibles for their healthcare but may have to make copayments depending on what procedure they are having. VHA is distinct from the U.S. Department of Defense Military Health System of which it is not a part.

A clinic is a health facility that is primarily focused on the care of outpatients. Clinics can be privately operated or publicly managed and funded. They typically cover the primary care needs of populations in local communities, in contrast to larger hospitals which offer more specialized treatments and admit inpatients for overnight stays.
Mental health in China is a growing issue. Experts have estimated that about 173 million people living in China are suffering from a mental disorder. The desire to seek treatment is largely hindered by China's strict social norms, as well as religious and cultural beliefs regarding personal reputation and social harmony.
Health care in Saudi Arabia is a national health care system in which the government provides free universal healthcare coverage through a number of government agencies. There is also a growing role and increased participation from the private sector in the provision of health care services. Saudi Arabia has been ranked among the 26 best countries in providing high quality healthcare.

The healthcare delivery system of Pakistan is complex because it includes healthcare subsystems by federal governments and provincial governments competing with formal and informal private sector healthcare systems. Healthcare is delivered mainly through vertically managed disease-specific mechanisms. The different institutions that are responsible for this include: provincial and district health departments, parastatal organizations, social security institutions, non-governmental organizations (NGOs) and private sector. The country's health sector is also marked by urban-rural disparities in healthcare delivery and an imbalance in the health workforce, with insufficient health managers, nurses, paramedics and skilled birth attendants in the peripheral areas. Pakistan's gross national income per capita in 2021 was $4,990 and the total expenditure on health per capita in 2021 was Rs 657.2 Billions, constituting 1.4% of the country's GDP. The health care delivery system in Pakistan consists of public and private sectors. Under the constitution, health is primarily responsibility of the provincial government, except in the federally administrated areas. Health care delivery has traditionally been jointly administered by the federal and provincial governments with districts mainly responsible for implementation. Service delivery is being organized through preventive, promotive, curative and rehabilitative services. The curative and rehabilitative services are being provided mainly at the secondary and tertiary care facilities. Preventive and promotive services, on the other hand, are mainly provided through various national programs; and community health workers’ interfacing with the communities through primary healthcare facilities and outreach activities. The state provides healthcare through a three-tiered healthcare delivery system and a range of public health interventions. Some government/ semi government organizations like the armed forces, Sui Gas, WAPDA, Railways, Fauji Foundation, Employees Social Security Institution and NUST provide health service to their employees and their dependents through their own system, however, these collectively cover about 10% of the population. The private health sector constitutes a diverse group of doctors, nurses, pharmacists, traditional healers, drug vendors, as well as laboratory technicians, shopkeepers and unqualified practitioners.

The Madigan Army Medical Center, located on Joint Base Lewis-McChord just outside Lakewood, Washington, is a key component of the Madigan Healthcare System and one of the largest military hospitals on the West Coast of the United States.
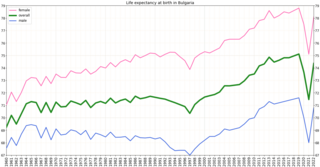
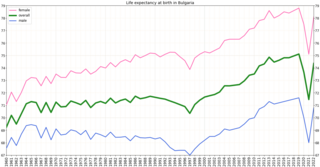
Bulgaria had the third highest mortality in Europe, at 708 per 100,000 population in 2015. The four European regions with the highest death rates from diseases of the circulatory system were all in Bulgaria. In the early 2000s, the major natural causes of death were cardiovascular disease, cancer, and respiratory illness. Bulgaria has had a very low incidence rate of human immunodeficiency virus (HIV). Although in 2003 the estimated rate of incidence was less than 0.1 percent of the population, in the early 2000s the number of new case reports increased annually. In 2005 some 86 new cases were reported, bringing the official total to about 600, and 58 new cases were reported in the first half of 2006. In 2010, there were 1,160 HIV-positive persons.
Health in Iraq refers to the country's public healthcare system and the overall health of the country's population. Iraq belongs to WHO health region Eastern Mediterranean and classified as upper middle according to World Bank income classification 2013. The state of health in Iraq has fluctuated during its turbulent recent history and specially during the last 4 decade. The country had one of the highest medical standards in the region during the period of 1980s and up until 1991, the annual total health budget was about $450 million in average. The 1991 Gulf War incurred Iraq's major infrastructures a huge damage. This includes health care system, sanitation, transport, water and electricity supplies. UN economic sanctions aggravated the process of deterioration. The annual total health budget for the country, a decade after the sanctions had fallen to $22 million which is barely 5% of what it was in 1980s. During its last decade, the regime of Saddam Hussein cut public health funding by 90 percent, contributing to a substantial deterioration in health care. During that period, maternal mortality increased nearly threefold, and the salaries of medical personnel decreased drastically. Medical facilities, which in 1980 were among the best in the Middle East, deteriorated. Conditions were especially serious in the south, where malnutrition and water-borne diseases became common in the 1990s. Health indicators deteriorated during the 1990s. In the late 1990s, Iraq's infant mortality rates more than doubled. Because treatment and diagnosis of cancer and diabetes decreased in the 1990s, complications and deaths resulting from those diseases increased drastically in the late 1990s and early 2000s.

The Healthcare in Kazakhstan is a post-Soviet healthcare system under reform. The World Health Organization (WHO), in 2000, ranked the Kazakhstani healthcare system as the 64th in overall performance, and 135th by overall level of health.
The Massachusetts General Hospital Psychiatry Academy is an educational organization for psychiatrists, psychologists, other mental health professionals, and other healthcare professionals who diagnose and treat patients with mental health disorders. It is directly organized and managed by the Department of Psychiatry at Massachusetts General Hospital, which is owned by Mass General Brigham, the largest healthcare provider in Massachusetts.

Mater Health Services North Queensland operates two private hospitals, one established by the Sisters of Mercy in 1945 named Mater Hospital Pimlico and the second purchased in 2007 named the Mater Women's and Children's Hospital Hyde Park.
Healthcare in Georgia is provided by a universal health care system under which the state funds medical treatment in a mainly privatized system of medical facilities. In 2013, the enactment of a universal health care program triggered universal coverage of government-sponsored medical care of the population and improving access to health care services. Responsibility for purchasing publicly financed health services lies with the Social Service Agency (SSA).

Healthcare in Serbia is delivered by means of a universal health care system.
This article provides a brief overview of the health care systems of the world, sorted by continent.
A moral injury is an injury to an individual's moral conscience and values resulting from an act of perceived moral transgression on the part of themselves or others, which produces profound feelings of guilt or shame—and in some cases a profound sense of betrayal and anger toward colleagues, commanders, the organization, politics, or society at large—moral disorientation, and societal alienation.
Operational stress injury or OSI is a non-clinical, non-medical term referring to a persistent psychological difficulty caused by traumatic experiences or prolonged high stress or fatigue during service as a military member or first responder. The term does not replace any individual diagnoses or disorders, but rather describes a category of mental health concerns linked to the particular challenges that these military members or first responders encounter in their service. There is not yet a single fixed definition. The term was first conceptualized within the Canadian Armed Forces to help foster understanding of the broader mental health challenges faced by military members who have been impacted by traumatic experiences and who face difficulty as a result. OSI encompasses a number of the diagnoses found in the Diagnostic and Statistical Manual of Mental Disorders (DSM) classification system, with the common thread being a linkage to the operational experiences of the afflicted. The term has gained traction outside of the military community as an appropriate way to describe similar challenges suffered by those whose work regularly exposes them to trauma, particularly front line emergency first responders such as but not limited to police, firefighters, paramedics, correctional officers, and emergency dispatchers. The term, at present mostly used within Canada, is increasingly significant in the development of legislation, policy, treatments and benefits in the military and first responder communities.

The Minneapolis Veterans Affairs Health Care System (VAHCS) is network of hospital and outpatient clinics based in Minneapolis, Minnesota, USA. It belongs to the VISN23 VA Midwest Health Care Network managed by the Veterans Health Administration of the Department of Veterans Affairs. The Minneapolis VAHCS provides healthcare for United States military veterans in areas such as medicine, surgery, psychiatry, physical medicine and rehabilitation, neurology, oncology, dentistry, geriatrics and extended care. As a teaching hospital, it operates comprehensive training programs for multiple treatment specialties. The Minneapolis VAHCS also hosts one of the largest research programs of any VA health care system and maintains research affiliations with the University of Minnesota.

The COVID-19 pandemic has impacted the mental health of people across the globe. The pandemic has caused widespread anxiety, depression, and post-traumatic stress disorder symptoms. According to the UN health agency WHO, in the first year of the COVID-19 pandemic, prevalence of common conditions such as depression and anxiety, went up by more than 25 per cent. The pandemic has damaged social relationships, trust in institutions and in other people, has caused changes in work and income, and has imposed a substantial burden of anxiety and worry on the population. Women and young people face the greatest risk of depression and anxiety.
The impact of the COVID-19 pandemic on hospitals became severe for some hospital systems of the United States in the spring of 2020, a few months after the COVID-19 pandemic began. Some had started to run out of beds, along with having shortages of nurses and doctors. By November 2020, with 13 million cases so far, hospitals throughout the country had been overwhelmed with record numbers of COVID-19 patients. Nursing students had to fill in on an emergency basis, and field hospitals were set up to handle the overflow.