Parathyroid hormone (PTH), also called parathormone or parathyrin, is a peptide hormone secreted by the parathyroid glands that regulates the serum calcium concentration through its effects on bone, kidney, and intestine.

Calcium metabolism is the movement and regulation of calcium ions (Ca2+) in (via the gut) and out (via the gut and kidneys) of the body, and between body compartments: the blood plasma, the extracellular and intracellular fluids, and bone. Bone acts as a calcium storage center for deposits and withdrawals as needed by the blood via continual bone remodeling.
Hypercalcemia, also spelled hypercalcaemia, is a high calcium (Ca2+) level in the blood serum. The normal range is 2.1–2.6 mmol/L (8.8–10.7 mg/dL, 4.3–5.2 mEq/L), with levels greater than 2.6 mmol/L defined as hypercalcemia. Those with a mild increase that has developed slowly typically have no symptoms. In those with greater levels or rapid onset, symptoms may include abdominal pain, bone pain, confusion, depression, weakness, kidney stones or an abnormal heart rhythm including cardiac arrest.
Disorders of calcium metabolism occur when the body has too little or too much calcium. The serum level of calcium is closely regulated within a fairly limited range in the human body. In a healthy physiology, extracellular calcium levels are maintained within a tight range through the actions of parathyroid hormone, vitamin D and the calcium sensing receptor. Disorders in calcium metabolism can lead to hypocalcemia, decreased plasma levels of calcium or hypercalcemia, elevated plasma calcium levels.
Hypoparathyroidism is decreased function of the parathyroid glands with underproduction of parathyroid hormone (PTH). This can lead to low levels of calcium in the blood, often causing cramping and twitching of muscles or tetany, and several other symptoms. It is a very rare disease. The condition can be inherited, but it is also encountered after thyroid or parathyroid gland surgery, and it can be caused by immune system-related damage as well as a number of rarer causes. The diagnosis is made with blood tests, and other investigations such as genetic testing depending on the results. The primary treatment of hypoparathyroidism is calcium and vitamin D supplementation. Calcium replacement or vitamin D can ameliorate the symptoms but can increase the risk of kidney stones and chronic kidney disease. Additionally, medications such as recombinant human parathyroid hormone or teriparatide may be given by injection to replace the missing hormone.

Hyperparathyroidism is an increase in parathyroid hormone (PTH) levels in the blood. This occurs from a disorder either within the parathyroid glands or as response to external stimuli. Symptoms of hyperparathyroidism are caused by inappropriately normal or elevated blood calcium excreted from the bones and flowing into the blood stream in response to increased production of parathyroid hormone. In healthy people, when blood calcium levels are high, parathyroid hormone levels should be low. With long-standing hyperparathyroidism, the most common symptom is kidney stones. Other symptoms may include bone pain, weakness, depression, confusion, and increased urination. Both primary and secondary may result in osteoporosis.

Dystrophic calcification (DC) is the calcification occurring in degenerated or necrotic tissue, as in hyalinized scars, degenerated foci in leiomyomas, and caseous nodules. This occurs as a reaction to tissue damage, including as a consequence of medical device implantation. Dystrophic calcification can occur even if the amount of calcium in the blood is not elevated, in contrast to metastatic calcification, which is a consequence of a systemic mineral imbalance, including hypercalcemia and/or hyperphosphatemia, that leads to calcium deposition in healthy tissues. In dystrophic calcification, basophilic calcium salt deposits aggregate, first in the mitochondria, then progressively throughout the cell. These calcifications are an indication of previous microscopic cell injury, occurring in areas of cell necrosis when activated phosphatases bind calcium ions to phospholipids in the membrane.

Parathyroidectomy is the surgical removal of one or more of the (usually) four parathyroid glands. This procedure is used to remove an adenoma or hyperplasia of these glands when they are producing excessive parathyroid hormone (PTH): hyperparathyroidism. The glands are usually four in number and located adjacent to the posterior surface of the thyroid gland, but their exact location is variable. When an elevated PTH level is found, a sestamibi scan or an ultrasound may be performed in order to confirm the presence and location of abnormal parathyroid tissue.
Renal osteodystrophy is currently defined as an alteration of bone morphology in patients with chronic kidney disease (CKD). It is one measure of the skeletal component of the systemic disorder of chronic kidney disease-mineral and bone disorder (CKD-MBD). The term "renal osteodystrophy" was coined in 1943, 60 years after an association was identified between bone disease and kidney failure.

Calcification is the accumulation of calcium salts in a body tissue. It normally occurs in the formation of bone, but calcium can be deposited abnormally in soft tissue, causing it to harden. Calcifications may be classified on whether there is mineral balance or not, and the location of the calcification. Calcification may also refer to the processes of normal mineral deposition in biological systems, such as the formation of stromatolites or mollusc shells.

Primary hyperparathyroidism is a medical condition where the parathyroid gland produce excess amounts of parathyroid hormone (PTH). The symptoms of the condition relate to the resulting elevated serum calcium (hypercalcemia), which can cause digestive symptoms, kidney stones, psychiatric abnormalities, and bone disease.
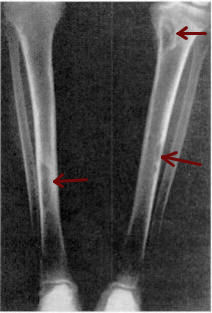
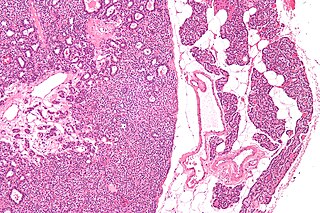
Osteitis fibrosa cystica is a skeletal disorder resulting in a loss of bone mass, a weakening of the bones as their calcified supporting structures are replaced with fibrous tissue, and the formation of cyst-like brown tumors in and around the bone. Osteitis fibrosis cystica (OFC), also known as osteitis fibrosa, osteodystrophia fibrosa, and von Recklinghausen's disease of bone, is caused by hyperparathyroidism, which is a surplus of parathyroid hormone from over-active parathyroid glands. This surplus stimulates the activity of osteoclasts, cells that break down bone, in a process known as osteoclastic bone resorption. The hyperparathyroidism can be triggered by a parathyroid adenoma, hereditary factors, parathyroid carcinoma, or renal osteodystrophy. Osteoclastic bone resorption releases minerals, including calcium, from the bone into the bloodstream, causing both elevated blood calcium levels, and the structural changes which weaken the bone. The symptoms of the disease are the consequences of both the general softening of the bones and the excess calcium in the blood, and include bone fractures, kidney stones, nausea, moth-eaten appearance in the bones, appetite loss, and weight loss.

Secondary hyperparathyroidism is the medical condition of excessive secretion of parathyroid hormone (PTH) by the parathyroid glands in response to hypocalcemia, with resultant hyperplasia of these glands. This disorder is primarily seen in patients with chronic kidney failure. It is sometimes abbreviated "SHPT" in medical literature.

Tertiary hyperparathyroidism is a condition involving the overproduction of the hormone, parathyroid hormone, produced by the parathyroid glands. The parathyroid glands are involved in monitoring and regulating blood calcium levels and respond by either producing or ceasing to produce parathyroid hormone.

Milk-alkali syndrome (MAS), also referred to as calcium-alkali syndrome, is the third most common cause of hypercalcemia. Milk-alkali syndrome is characterized by elevated blood calcium levels, metabolic alkalosis, and acute kidney injury.

Ectopic calcification is a pathologic deposition of calcium salts in tissues or bone growth in soft tissues. This can be a symptom of hyperphosphatemia. Formation of osseous tissue in soft tissues such as the lungs, eyes, arteries, or other organs is known as ectopic calcification, dystrophic calcification, or ectopic ossification.
Many conditions are associated with disorders of the function of the parathyroid gland. Some disorders may be purely anatomical resulting in an enlarged gland which will raise concern. Such benign disorders, such as parathyroid cyst, are not discussed here. Parathyroid diseases can be divided into those causing hyperparathyroidism, and those causing hypoparathyroidism.
Familial hypocalciuric hypercalcemia (FHH) is an inherited condition that can cause hypercalcemia, a serum calcium level typically above 10.2 mg/dL; although uncommon. It is also known as familial benign hypocalciuric hypercalcemia (FBHH) where there is usually a family history of hypercalcemia which is mild, a urine calcium to creatinine ratio <0.01, and urine calcium <200 mg/day (hypocalciuria).
Recombinant human parathyroid hormone, sold under the brand name Preotact among others, is an artificially manufactured form of the parathyroid hormone used to treat hypoparathyroidism. Recombinant human parathyroid hormone is used in the treatment of osteoporosis in postmenopausal women at high risk of osteoporotic fractures. A significant reduction in the incidence of vertebral fractures has been demonstrated. It is used in combination with calcium and vitamin D supplements.
Chronic kidney disease–mineral and bone disorder (CKD–MBD) is one of the many complications associated with chronic kidney disease. It represents a systemic disorder of mineral and bone metabolism due to CKD manifested by either one or a combination of the following: