Related Research Articles

An antibiotic is a type of antimicrobial substance active against bacteria. It is the most important type of antibacterial agent for fighting bacterial infections, and antibiotic medications are widely used in the treatment and prevention of such infections. They may either kill or inhibit the growth of bacteria. A limited number of antibiotics also possess antiprotozoal activity. Antibiotics are not effective against viruses such as the common cold or influenza; drugs which inhibit growth of viruses are termed antiviral drugs or antivirals rather than antibiotics. They are also not effective against fungi; drugs which inhibit growth of fungi are called antifungal drugs.

Antimicrobial resistance (AMR) occurs when microbes evolve mechanisms that protect them from the effects of antimicrobials. All classes of microbes can evolve resistance. Fungi evolve antifungal resistance. Viruses evolve antiviral resistance. Protozoa evolve antiprotozoal resistance, and bacteria evolve antibiotic resistance. Those bacteria that are considered extensively drug resistant (XDR) or totally drug-resistant (TDR) are sometimes called "superbugs". Although antimicrobial resistance is a naturally-occurring process, it is often the result of improper usage of the drugs and management of the infections.

Drug resistance is the reduction in effectiveness of a medication such as an antimicrobial or an antineoplastic in treating a disease or condition. The term is used in the context of resistance that pathogens or cancers have "acquired", that is, resistance has evolved. Antimicrobial resistance and antineoplastic resistance challenge clinical care and drive research. When an organism is resistant to more than one drug, it is said to be multidrug-resistant.
An antimicrobial is an agent that kills microorganisms or stops their growth. Antimicrobial medicines can be grouped according to the microorganisms they act primarily against. For example, antibiotics are used against bacteria, and antifungals are used against fungi. They can also be classified according to their function. Agents that kill microbes are microbicides, while those that merely inhibit their growth are called bacteriostatic agents. The use of antimicrobial medicines to treat infection is known as antimicrobial chemotherapy, while the use of antimicrobial medicines to prevent infection is known as antimicrobial prophylaxis.

Carbapenems are a class of very effective antibiotic agents most commonly used for the treatment of severe bacterial infections. This class of antibiotics is usually reserved for known or suspected multidrug-resistant (MDR) bacterial infections. Similar to penicillins and cephalosporins, carbapenems are members of the beta lactam class of antibiotics, which kill bacteria by binding to penicillin-binding proteins, thus inhibiting bacterial cell wall synthesis. However, these agents individually exhibit a broader spectrum of activity compared to most cephalosporins and penicillins. Furthermore, carbapenems are typically unaffected by emerging antibiotic resistance, even to other beta-lactams.
Production of antibiotics is a naturally occurring event, that thanks to advances in science can now be replicated and improved upon in laboratory settings. Due to the discovery of penicillin by Alexander Flemming, and the efforts of Florey and Chain in 1938, large-scale, pharmaceutical production of antibiotics has been made possible. As with the initial discovery of penicillin, most antibiotics have been discovered as a result of happenstance. Antibiotic production can be grouped into three methods: natural fermentation, semi-synthetic, and synthetic. As more and more bacteria continue to develop resistance to currently produced antibiotics, research and development of new antibiotics continues to be important. In addition to research and development into the production of new antibiotics, repackaging delivery systems is important to improving efficacy of the antibiotics that are currently produced. Improvements to this field have seen the ability to add antibiotics directly into implanted devices, aerosolization of antibiotics for direct delivery, and combination of antibiotics with non antibiotics to improve outcomes. The increase of antibiotic resistant strains of pathogenic bacteria has led to an increased urgency for the funding of research and development of antibiotics and a desire for production of new and better acting antibiotics.

Antibiotic sensitivity testing or antibiotic susceptibility testing is the measurement of the susceptibility of bacteria to antibiotics. It is used because bacteria may have resistance to some antibiotics. Sensitivity testing results can allow a clinician to change the choice of antibiotics from empiric therapy, which is when an antibiotic is selected based on clinical suspicion about the site of an infection and common causative bacteria, to directed therapy, in which the choice of antibiotic is based on knowledge of the organism and its sensitivities.
In microbiology, the minimum inhibitory concentration (MIC) is the lowest concentration of a chemical, usually a drug, which prevents visible growth of a bacterium or bacteria. MIC depends on the microorganism, the affected human being, and the antibiotic itself. It is often expressed in micrograms per milliliter (μg/mL) or milligrams per liter (mg/L).

The disk diffusion test is a culture-based microbiology assay used in diagnostic and drug discovery laboratories. In diagnostic labs, the assay is used to determine the susceptibility of bacteria isolated from a patient's infection to clinically approved antibiotics. This allows physicians to prescribe the most appropriate antibiotic treatment. In drug discovery labs, especially bioprospecting labs, the assay is used to screen biological material and drug candidates for antibacterial activity. When bioprospecting, the assay can be performed with paired strains of bacteria to achieve dereplication and provisionally identify antibacterial mechanism of action.

Medical microbiology, the large subset of microbiology that is applied to medicine, is a branch of medical science concerned with the prevention, diagnosis and treatment of infectious diseases. In addition, this field of science studies various clinical applications of microbes for the improvement of health. There are four kinds of microorganisms that cause infectious disease: bacteria, fungi, parasites and viruses, and one type of infectious protein called prion.

Novozymes A/S is a global biotechnology company headquartered in Bagsværd outside of Copenhagen, Denmark. The company's focus is the research, development and production of industrial enzymes, microorganisms, and biopharmaceutical ingredients.
Cubist Pharmaceuticals was an American biopharmaceutical company that targeted pathogens like MRSA.
Teixobactin is a peptide-like secondary metabolite of some species of bacteria, that kills some gram-positive bacteria. It appears to belong to a new class of antibiotics, and harms bacteria by binding to lipid II and lipid III, important precursor molecules for forming the cell wall.
Eleftheria terrae is a recently discovered Gram-negative bacterium. E. terrae is a temporary name for the organism, as it was only discovered in 2014 and is still undergoing scientific study. It was found to produce a previously unknown antibiotic named teixobactin. The discovery of E. terrae could represent a new age of antibiotics, as teixobactin is the first new antibiotic discovered since the synthetic era of the 1980s. Prior research has indicated that other uncultivable bacteria like E. terrae have potential in the development of new antimicrobial agents.

Enduracididine is a non-proteinogenic α-amino acid that is a cyclic analogue of arginine. It is not genetically encoded into peptide sequences, but rather is generated as a posttranslational modification.
The Isolation chip is a method of culturing bacteria. Using regular methods, 99% of bacterial species are not able to be cultured as they do not grow in conditions made in a laboratory, a problem called the "Great Plate Count Anomaly". The ichip instead cultures bacterial species within its soil environment. The soil is diluted in molten agar and nutrients such that only a single cell, on average, grows in the ichip's small compartments or wells, hence the term "isolation". The chip is then enclosed in a semipermeable plastic membrane and buried back in the dirt to allow in nutrients not available in the lab. With this culturing method, about 50 to 60 percent of bacterial species are able to survive. Notably, the bacterial species Eleftheria terrae, which makes the antibiotic teixobactin that has shown promise against many drug-resistant strains like methicillin-resistant Staphylococcus aureus, was discovered using the ichip in 2015. In addition to antibiotics, it is argued that anti-cancer agents, anti-inflammatory and immunosuppressives as well as potential energy sources could be discovered. The ichip was developed by the drug discovery company NovoBiotic Pharmaceuticals, founded by Kim Lewis and Slava Epstein.
Antivirulence is the concept of blocking virulence factors. In regards to bacteria, the idea is to design agents that block virulence rather than kill bacteria en masse, as the current regime results in much more selective pressure.
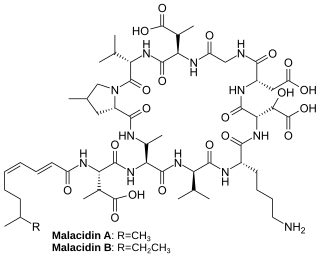
Malacidins are a class of chemicals made by bacteria found in soil that can kill Gram-positive bacteria. Their activity appears to be dependent on calcium. The discovery of malacidins was published in 2018.
Kim Lewis is an American researcher, author and academic. He is a University Distinguished Professor and the director of Antimicrobial Discovery Center at Northeastern University.
Slava Epstein is an American academic, researcher and entrepreneur working in the field of Microbial ecology. He is currently a professor in the biology department of Northeastern University and co-founder of NovoBiotic Pharmaceuticals. As a researcher his most covered contribution is the development of the Isolation chip (iChip) and the discovery of a new antibiotic, Teixobactin. Epstein's research has been published in many leading scientific journals including Nature and Science.
References
- ↑ Khatchadourian, Raffi (20 June 2016). "The Unseen: Millions of microbes are yet to be discovered. Will one hold the ultimate cure?". The New Yorker. New York: Condé Nast. Retrieved 27 June 2016.
- 1 2 Denise, Grady. "From a Pile of Dirt, Hope for a Powerful New Antibiotic". The New York Times . Retrieved 7 January 2015.
- ↑ WO 2014089053,"Novel depsipeptide and uses thereof",published 12 June 2014, assigned to Novobiotic Pharmaceuticals LLC [US]
- ↑ Ling, Losee; Schneider, Tanja; Peoples, Aaron; Spoering, Amy; Engels, Ina; Conlon, Brian; Mueller, Anna; Schäberle, Till; Hughes, Dallas; Epstein, Slava; Jones, Michael; Lazarides, Linos; Steadman, Victoria; Cohen, Douglas; Felix, Cintia; Fetterman, K. Ashley; Millett, William; Nitti, Anthony; Zullo, Ashley; Chen, Chao; Lewis, Kim (7 January 2015). "A new antibiotic kills pathogens without detectable resistance". Nature . 517 (7535): 455–9. doi:10.1038/nature14098. PMC 7414797 . PMID 25561178.
- ↑ Lewis, Kim (7 January 2015). "NovoBiotic reports the discovery of teixobactin, a new antibiotic without detectable resistance" (PDF). Cambridge, MA (USA): NovoBiotic Pharmaceuticals. Retrieved 7 January 2015.
- 1 2 Gallagher, James (7 January 2015). "Antibiotics: US discovery labelled 'game-changer' for medicine". BBC. Retrieved 7 January 2015.