An antacid is a substance which neutralizes stomach acidity and is used to relieve heartburn, indigestion or an upset stomach. Some antacids have been used in the treatment of constipation and diarrhea. Marketed antacids contain salts of aluminium, calcium, magnesium, or sodium. Some preparations contain a combination of two salts, such as magnesium carbonate and aluminium hydroxide.
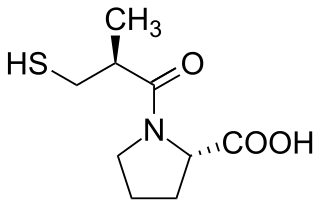
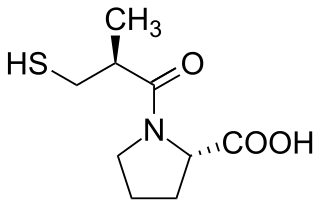
Angiotensin-converting-enzyme inhibitors are a class of medication used primarily for the treatment of high blood pressure and heart failure. This class of medicine works by causing relaxation of blood vessels as well as a decrease in blood volume, which leads to lower blood pressure and decreased oxygen demand from the heart.

Allopurinol is a medication used to decrease high blood uric acid levels. It is specifically used to prevent gout, prevent specific types of kidney stones and for the high uric acid levels that can occur with chemotherapy. It is taken by mouth or injected into a vein.

Amitriptyline, sold under the brand name Elavil among others, is a tricyclic antidepressant primarily used to treat major depressive disorder, a variety of pain syndromes such as neuropathic pain, fibromyalgia, migraine and tension headaches. Due to the frequency and prominence of side effects, amitriptyline is generally considered a second-line therapy for these indications.
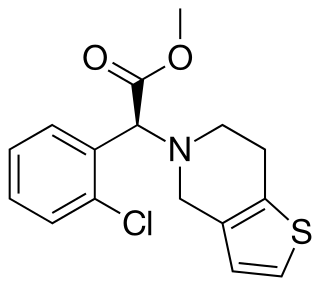
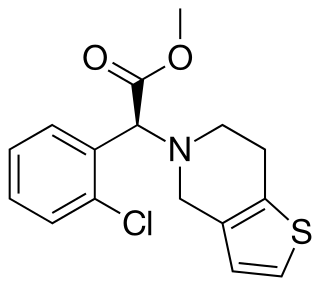
Clopidogrel — sold under the brand name Plavix, among others — is an antiplatelet medication used to reduce the risk of heart disease and stroke in those at high risk. It is also used together with aspirin in heart attacks and following the placement of a coronary artery stent. It is taken by mouth. Its effect starts about two hours after intake and lasts for five days.
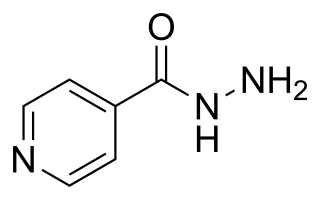
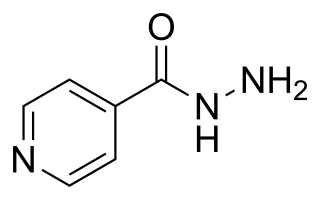
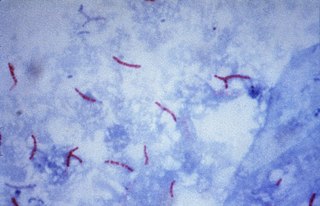
Isoniazid, also known as isonicotinic acid hydrazide (INH), is an antibiotic used for the treatment of tuberculosis. For active tuberculosis, it is often used together with rifampicin, pyrazinamide, and either streptomycin or ethambutol. For latent tuberculosis, it is often used alone. It may also be used for atypical types of mycobacteria, such as M. avium, M. kansasii, and M. xenopi. It is usually taken by mouth, but may be used by injection into muscle.
Antihypertensives are a class of drugs that are used to treat hypertension. Antihypertensive therapy seeks to prevent the complications of high blood pressure, such as stroke, heart failure, kidney failure and myocardial infarction. Evidence suggests that reduction of the blood pressure by 5 mmHg can decrease the risk of stroke by 34% and of ischaemic heart disease by 21%, and can reduce the likelihood of dementia, heart failure, and mortality from cardiovascular disease. There are many classes of antihypertensives, which lower blood pressure by different means. Among the most important and most widely used medications are thiazide diuretics, calcium channel blockers, ACE inhibitors, angiotensin II receptor antagonists (ARBs), and beta blockers.
Atenolol is a beta blocker medication primarily used to treat high blood pressure and heart-associated chest pain. Atenolol, however, does not seem to improve mortality in those with high blood pressure. Other uses include the prevention of migraines and treatment of certain irregular heart beats. It is taken by mouth or by injection into a vein. It can also be used with other blood pressure medications.

Abacavir, sold under the brand name Ziagen among others, is a medication used to treat HIV/AIDS. Similar to other nucleoside analog reverse-transcriptase inhibitors (NRTIs), abacavir is used together with other HIV medications, and is not recommended by itself. It is taken by mouth as a tablet or solution and may be used in children over the age of three months.

Pharmacogenomics is the study of the role of the genome in drug response. Its name reflects its combining of pharmacology and genomics. Pharmacogenomics analyzes how the genetic makeup of a patient affects their response to drugs. It deals with the influence of acquired and inherited genetic variation on drug response, by correlating DNA mutations with pharmacokinetic, pharmacodynamic, and/or immunogenic endpoints.
Polypharmacy (polypragmasia) is an umbrella term to describe the simultaneous use of multiple medicines by a patient for their conditions. Most commonly it is defined as regularly taking five or more medicines but definitions vary in where they draw the line for the minimum number of drugs. Polypharmacy is often the consequence of having multiple long-term conditions, also known as multimorbidity. An excessive number of medications is worrisome, especially for older patients with many chronic health conditions, because this increases the risk of an adverse event in those patients.
Omalizumab, sold under the brand name Xolair, is a medication used to treat asthma, nasal polyps, and urticaria (hives).

Tuberculosis management describes the techniques and procedures utilized for treating tuberculosis (TB).
An adverse effect is an undesired harmful effect resulting from a medication or other intervention, such as surgery. An adverse effect may be termed a "side effect", when judged to be secondary to a main or therapeutic effect. The term complication is similar to adverse effect, but the latter is typically used in pharmacological contexts, or when the negative effect is expected or common. If the negative effect results from an unsuitable or incorrect dosage or procedure, this is called a medical error and not an adverse effect. Adverse effects are sometimes referred to as "iatrogenic" because they are generated by a physician/treatment. Some adverse effects occur only when starting, increasing or discontinuing a treatment. Adverse effects can also be caused by placebo treatments . Using a drug or other medical intervention which is contraindicated may increase the risk of adverse effects. Adverse effects may cause complications of a disease or procedure and negatively affect its prognosis. They may also lead to non-compliance with a treatment regimen. Adverse effects of medical treatment resulted in 142,000 deaths in 2013 up from 94,000 deaths in 1990 globally.
Combination therapy or polytherapy is therapy that uses more than one medication or modality. Typically, the term refers to using multiple therapies to treat a single disease, and often all the therapies are pharmaceutical. 'Pharmaceutical' combination therapy may be achieved by prescribing/administering separate drugs, or, where available, dosage forms that contain more than one active ingredient.
In medicine, patient compliance describes the degree to which a patient correctly follows medical advice. Most commonly, it refers to medication or drug compliance, but it can also apply to other situations such as medical device use, self care, self-directed exercises, or therapy sessions. Both patient and health-care provider affect compliance, and a positive physician-patient relationship is the most important factor in improving compliance. Access to care plays a role in patient adherence, whereby greater wait times to access care contributing to greater absenteeism. The cost of prescription medication also plays a major role.
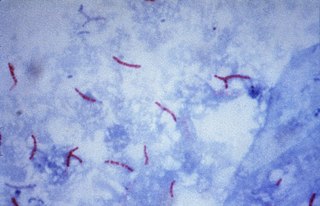
Multidrug-resistant tuberculosis (MDR-TB) is a form of tuberculosis (TB) infection caused by bacteria that are resistant to treatment with at least two of the most powerful first-line anti-TB medications (drugs): isoniazid and rifampin. Some forms of TB are also resistant to second-line medications, and are called extensively drug-resistant TB (XDR-TB).

Brivaracetam, sold under the brand name Briviact among others, is a chemical analog of levetiracetam, is a racetam derivative with anticonvulsant (antiepileptic) properties. It is marketed by the pharmaceutical company UCB.
Treatment as prevention (TasP) is a concept in public health that promotes treatment as a way to prevent and reduce the likelihood of HIV illness, death and transmission from an infected individual to others. Expanding access to earlier HIV diagnosis and treatment as a means to address the global epidemic by preventing illness, death and transmission was first proposed in 2000 by Garnett et al. The term is often used to talk about treating people that are currently living with human immunodeficiency virus (HIV) and acquired immune deficiency syndrome (AIDS) to prevent illness, death and transmission. Although some experts narrow this to only include preventing infections, treatment prevents illnesses such as tuberculosis and has been shown to prevent death. The dual impact on well-being and its 100% effectiveness in reducing transmission makes TasP the most important element in the HIV prevention toolkit. In relation to HIV, antiretroviral therapy (ART) is a three or more drug combination therapy that is used to decrease the viral load, or the measured amount of virus, in an infected individual. Such medications are used as a preventative for infected individuals to not only spread the HIV virus to their negative partners but also improve their current health to increase their lifespans. Other names for ART include highly active antiretroviral therapy (HAART), combination antiretroviral therapy (cART), triple therapy and triple drug cocktail. When taken correctly, ART is able to diminish the presence of the HIV virus in the bodily fluids of an infected person to a level of undetectability. Undetectability ensures that infection does not necessarily have an effect on a person's general health, and that there is no longer a risk of passing along HIV to others. Consistent adherence to an ARV regimen, monitoring, and testing are essential for continued confirmed viral suppression. Treatment as prevention rose to great prominence in 2011, as part of the HPTN 052 study, which shed light on the benefits of early treatment for HIV positive individuals.
Additive effect in pharmacology describes the situation when the combining effects of two drugs equal the sum of the effects of the two drugs acting independently. The concept of additive effect is derived from the concept of synergy. It was introduced by the scientists in pharmacology and biochemistry fields in the process of understanding the synergistic interaction between drugs and chemicals over the century.