Ramsay Hunt syndrome type 2, commonly referred to simply as Ramsay Hunt syndrome (RHS) and also known as herpes zoster oticus, is inflammation of the geniculate ganglion of the facial nerve as a late consequence of varicella zoster virus (VZV). In regard to the frequency, less than 1% of varicella zoster infections involve the facial nerve and result in RHS. It is traditionally defined as a triad of ipsilateral facial paralysis, otalgia, and vesicles close to the ear and auditory canal. Due to its proximity to the vestibulocochlear nerve, the virus can spread and cause hearing loss, tinnitus, and vertigo. It is common for diagnoses to be overlooked or delayed, which can raise the likelihood of long-term consequences. It is more complicated than Bell's palsy. Therapy aims to shorten its overall length, while also providing pain relief and averting any consequences.

The parasympathetic nervous system (PSNS) is one of the three divisions of the autonomic nervous system, the others being the sympathetic nervous system and the enteric nervous system. The enteric nervous system is sometimes considered part of the autonomic nervous system, and sometimes considered an independent system.

The facial nerve, also known as the seventh cranial nerve, cranial nerve VII, or simply CN VII, is a cranial nerve that emerges from the pons of the brainstem, controls the muscles of facial expression, and functions in the conveyance of taste sensations from the anterior two-thirds of the tongue. The nerve typically travels from the pons through the facial canal in the temporal bone and exits the skull at the stylomastoid foramen. It arises from the brainstem from an area posterior to the cranial nerve VI and anterior to cranial nerve VIII.
Articles related to anatomy include:
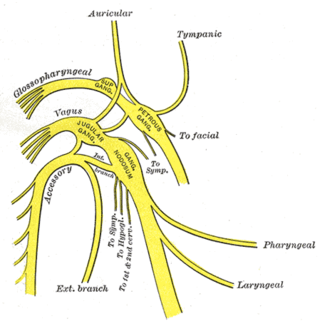
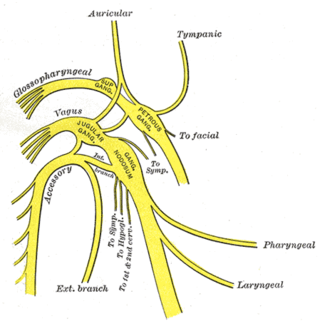
The glossopharyngeal nerve, also known as the ninth cranial nerve, cranial nerve IX, or simply CN IX, is a cranial nerve that exits the brainstem from the sides of the upper medulla, just anterior to the vagus nerve. Being a mixed nerve (sensorimotor), it carries afferent sensory and efferent motor information. The motor division of the glossopharyngeal nerve is derived from the basal plate of the embryonic medulla oblongata, whereas the sensory division originates from the cranial neural crest.
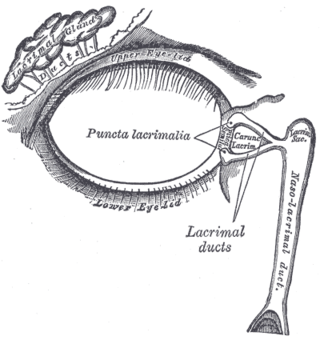
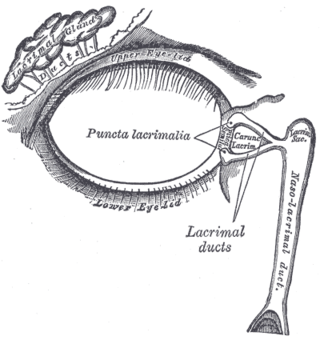
The lacrimal glands are paired exocrine glands, one for each eye, found in most terrestrial vertebrates and some marine mammals, that secrete the aqueous layer of the tear film. In humans, they are situated in the upper lateral region of each orbit, in the lacrimal fossa of the orbit formed by the frontal bone. Inflammation of the lacrimal glands is called dacryoadenitis. The lacrimal gland produces tears which are secreted by the lacrimal ducts, and flow over the ocular surface, and then into canals that connect to the lacrimal sac. From that sac, the tears drain through the lacrimal duct into the nose.

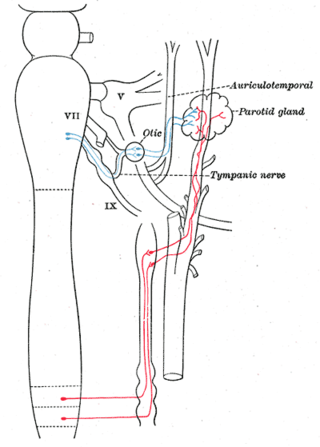
The otic ganglion is a small parasympathetic ganglion located immediately below the foramen ovale in the infratemporal fossa and on the medial surface of the mandibular nerve. It is functionally associated with the glossopharyngeal nerve and innervates the parotid gland for salivation.

The pterygopalatine ganglion is a parasympathetic ganglion in the pterygopalatine fossa. It is one of four parasympathetic ganglia of the head and neck,.
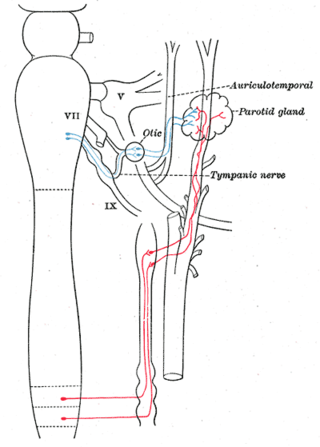
The auriculotemporal nerve is a sensory branch of the mandibular nerve (CN V3) that runs with the superficial temporal artery and vein, and provides sensory innervation to parts of the external ear, scalp, and temporomandibular joint. The nerve also conveys post-ganglionic parasympathetic fibres from the otic ganglion to the parotid gland.
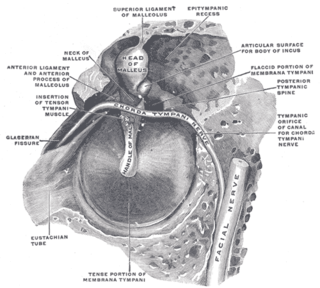
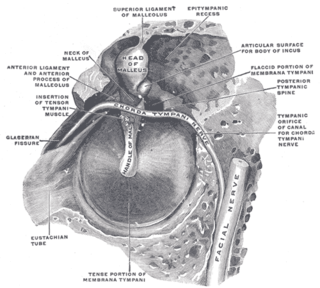
Chorda tympani is a branch of the facial nerve that carries gustatory (taste) sensory innervation from the front of the tongue and parasympathetic (secretomotor) innervation to the submandibular and sublingual salivary glands.

The greater petrosal nerve is a nerve of the head mainly containing pre-ganglionic parasympathetic fibres which ultimately synapse in the pterygopalatine ganglion. It branches from the facial nerve and is derived from the parasympathetic part of the nervus intermedius component of CN VII, with its cell bodies located in the superior salivary nucleus. In the connective tissue substance of the foramen lacerum, the greater petrosal nerve unites with the (sympathetic) deep petrosal nerve to form the nerve of the pterygoid canal which proceeds to the pterygopalatine ganglion.

The nasociliary nerve is a branch of the ophthalmic nerve (CN V1) (which is in turn a branch of the trigeminal nerve (CN V)). It is intermediate in size between the other two branches of the ophthalmic nerve, the frontal nerve and lacrimal nerve.

A jugular foramen is one of the two large foramina (openings) in the base of the skull, located behind the carotid canal. It is formed by the temporal bone and the occipital bone. It allows many structures to pass, including the inferior petrosal sinus, three cranial nerves, the sigmoid sinus, and meningeal arteries.

The internal auditory meatus is a canal within the petrous part of the temporal bone of the skull between the posterior cranial fossa and the inner ear.

The facial canal is a Z-shaped canal in the temporal bone of the skull. It extends between the internal acoustic meatus and stylomastoid foramen. It transmits the facial nerve.
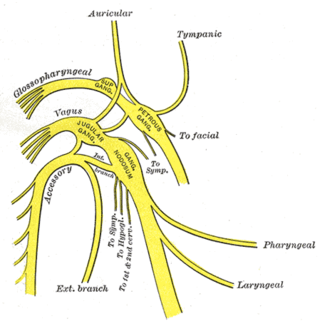
The tympanic nerve is a branch of the glossopharyngeal nerve found near the ear. It gives sensation to the middle ear, the Eustachian tube, the parotid gland, and mastoid air cells. It gives parasympathetic to supply to the parotid gland via the otic ganglion and the auriculotemporal nerve.

The lesser petrosal nerve is the general visceral efferent (GVE) nerve conveying pre-ganglionic parasympathetic secretomotor fibers for the parotid gland from the tympanic plexus to the otic ganglion. It passes out of the tympanic cavity through the petrous part of the temporal bone into the middle cranial fossa of the cranial cavity, then exits the cranial cavity through its own canaliculus to reach the infratemporal fossa.

The nerve of the pterygoid canal is formed by the union of the (parasympathetic) greater petrosal nerve and (sympathetic) deep petrosal nerve within the cartilaginous substance filling the foramen lacerum. From the foramen lacerum, the nerve of the pterygoid canal passes through the pterygoid canal to reach the pterygopalatine fossa, ending at the pterygopalatine ganglion.

The intermediate nerve, nervus intermedius, nerve of Wrisberg or glossopalatine nerve is the part of the facial nerve located between the motor component of the facial nerve and the vestibulocochlear nerve. It contains the sensory and parasympathetic fibers of the facial nerve. Upon reaching the facial canal, it joins with the motor root of the facial nerve at the geniculate ganglion. Alex Alfieri postulates that the intermediate nerve should be considered as a separate cranial nerve and not a part of the facial nerve.
Geniculate ganglionitis or geniculate neuralgia (GN), also called nervus intermedius neuralgia, Ramsay Hunt syndrome, or Hunt's neuralgia, is a rare disorder characterized by severe paroxysmal neuralgic pain deep in the ear, that may spread to the ear canal, outer ear, mastoid or eye regions. GN may also occur in combination with trigeminal or glossopharyngeal neuralgia.