The rhinovirus is a positive-sense, single-stranded RNA virus belonging to the genus Enterovirus in the family Picornaviridae. Rhinovirus is the most common viral infectious agent in humans and is the predominant cause of the common cold.

Rotaviruses are the most common cause of diarrhoeal disease among infants and young children. Nearly every child in the world is infected with a rotavirus at least once by the age of five. Immunity develops with each infection, so subsequent infections are less severe. Adults are rarely affected. Rotavirus is a genus of double-stranded RNA viruses in the family Reoviridae. There are nine species of the genus, referred to as A, B, C, D, F, G, H, I and J. Rotavirus A is the most common species, and these rotaviruses cause more than 90% of rotavirus infections in humans.
Paramyxoviridae is a family of negative-strand RNA viruses in the order Mononegavirales. Vertebrates serve as natural hosts. Diseases associated with this family include measles, mumps, and respiratory tract infections. The family has four subfamilies, 17 genera, three of which are unassigned to a subfamily, and 78 species.

Croup, also known as laryngotracheobronchitis, is a type of respiratory infection that is usually caused by a virus. The infection leads to swelling inside the trachea, which interferes with normal breathing and produces the classic symptoms of "barking/brassy" cough, inspiratory stridor and a hoarse voice. Fever and runny nose may also be present. These symptoms may be mild, moderate, or severe. Often it starts or is worse at night and normally lasts one to two days.

Adenoviruses are medium-sized, nonenveloped viruses with an icosahedral nucleocapsid containing a double-stranded DNA genome. Their name derives from their initial isolation from human adenoids in 1953.

Respiratory syncytial virus (RSV), also called human respiratory syncytial virus (hRSV) and human orthopneumovirus, is a contagious virus that causes infections of the respiratory tract. It is a negative-sense, single-stranded RNA virus. Its name is derived from the large cells known as syncytia that form when infected cells fuse.

Human metapneumovirus is a negative-sense single-stranded RNA virus of the family Pneumoviridae and is closely related to the Avian metapneumovirus (AMPV) subgroup C. It was isolated for the first time in 2001 in the Netherlands by using the RAP-PCR technique for identification of unknown viruses growing in cultured cells. As of 2016, it was the second most common cause of acute respiratory tract illness in otherwise-healthy children under the age of 5 in a large US outpatient clinic.
Coinfection is the simultaneous infection of a host by multiple pathogen species. In virology, coinfection includes simultaneous infection of a single cell by two or more virus particles. An example is the coinfection of liver cells with hepatitis B virus and hepatitis D virus, which can arise incrementally by initial infection followed by superinfection.
Viral pneumonia is a pneumonia caused by a virus. Pneumonia is an infection that causes inflammation in one or both of the lungs. The pulmonary alveoli fill with fluid or pus making it difficult to breathe. Pneumonia can be caused by bacteria, viruses, fungi or parasites. Viruses are the most common cause of pneumonia in children, while in adults bacteria are a more common cause.

Respiratory tract infections (RTIs) are infectious diseases involving the lower or upper respiratory tract. An infection of this type usually is further classified as an upper respiratory tract infection or a lower respiratory tract infection. Lower respiratory infections, such as pneumonia, tend to be far more severe than upper respiratory infections, such as the common cold.

Human coronavirus NL63 (HCoV-NL63) is a species of coronavirus, specifically a Setracovirus from among the Alphacoronavirus genus. It was identified in late 2004 in patients in the Netherlands by Lia van der Hoek and Krzysztof Pyrc using a novel virus discovery method VIDISCA. Later on the discovery was confirmed by the researchers from the Rotterdam, the Netherlands The virus is an enveloped, positive-sense, single-stranded RNA virus which enters its host cell by binding to ACE2. Infection with the virus has been confirmed worldwide, and has an association with many common symptoms and diseases. Associated diseases include mild to moderate upper respiratory tract infections, severe lower respiratory tract infection, croup and bronchiolitis.

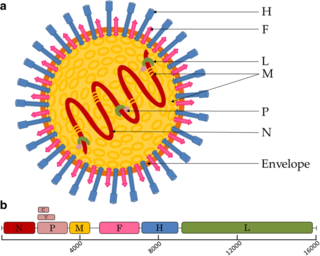
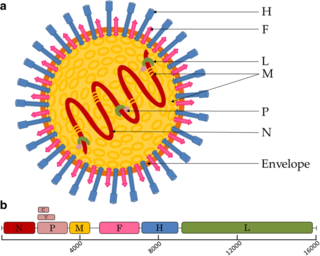
Murine respirovirus, formerly Sendai virus (SeV) and previously also known as murine parainfluenza virus type 1 or hemagglutinating virus of Japan (HVJ), is an enveloped, 150-200 nm–diameter, negative sense, single-stranded RNA virus of the family Paramyxoviridae. It typically infects rodents and it is not pathogenic for humans or domestic animals.
Palivizumab, sold under the brand name Synagis, is a monoclonal antibody produced by recombinant DNA technology used to prevent severe disease caused by respiratory syncytial virus (RSV) infections. It is recommended for infants at high-risk for RSV due to conditions such as prematurity or other medical problems including heart or lung diseases.

Antibody-dependent enhancement (ADE), sometimes less precisely called immune enhancement or disease enhancement, is a phenomenon in which binding of a virus to suboptimal antibodies enhances its entry into host cells, followed by its replication. The suboptimal antibodies can result from natural infection or from vaccination. ADE may cause enhanced respiratory disease, but is not limited to respiratory disease. It has been observed in HIV, RSV virus and Dengue virus and is monitored for in vaccine development.

A virus is a submicroscopic infectious agent that replicates only inside the living cells of an organism. Viruses infect all life forms, from animals and plants to microorganisms, including bacteria and archaea. Viruses are found in almost every ecosystem on Earth and are the most numerous type of biological entity. Since Dmitri Ivanovsky's 1892 article describing a non-bacterial pathogen infecting tobacco plants and the discovery of the tobacco mosaic virus by Martinus Beijerinck in 1898, more than 11,000 of the millions of virus species have been described in detail. The study of viruses is known as virology, a subspeciality of microbiology.

Influenza, commonly known as "the flu" or just "flu", is an infectious disease caused by influenza viruses. Symptoms range from mild to severe and often include fever, runny nose, sore throat, muscle pain, headache, coughing, and fatigue. These symptoms begin one to four days after exposure to the virus and last for about two to eight days. Diarrhea and vomiting can occur, particularly in children. Influenza may progress to pneumonia from the virus or a subsequent bacterial infection. Other complications include acute respiratory distress syndrome, meningitis, encephalitis, and worsening of pre-existing health problems such as asthma and cardiovascular disease.

Pneumoviridae is a family of negative-strand RNA viruses in the order Mononegavirales. Humans, cattle, and rodents serve as natural hosts. Respiratory tract infections are associated with member viruses such as human respiratory syncytial virus. There are five species in the family which are divided between the genera Metapneumovirus and Orthopneumovirus. The family used to be considered as a sub-family of Paramyxoviridae, but has been reclassified as of 2016.
A respiratory syncytial virus vaccine, or RSV vaccine, is a vaccine that protects against respiratory syncytial virus. RSV affects an estimated 64 million people and causes 160,000 deaths worldwide each year.

Jason S. McLellan is a structural biologist, professor in the Department of Molecular Biosciences and Robert A. Welch Chair in Chemistry at The University of Texas at Austin who specializes in understanding the structure and function of viral proteins, including those of coronaviruses. His research focuses on applying structural information to the rational design of vaccines and other therapies for viruses, including SARS-CoV-2, the novel coronavirus that causes COVID-19, and respiratory syncytial virus (RSV). McLellan and his team collaborated with researchers at the National Institute of Allergy and Infectious Diseases’ Vaccine Research Center to design a stabilized version of the SARS-CoV-2 spike protein, which biotechnology company Moderna used as the basis for the vaccine mRNA-1273, the first COVID-19 vaccine candidate to enter phase I clinical trials in the U.S. At least three other vaccines use this modified spike protein: those from Pfizer and BioNTech; Johnson & Johnson and Janssen Pharmaceuticals; and Novavax.
Bovine respiratory syncytial virus (BRSV) is pneumovirus closely related to human respiratory syncytial virus (RSV) that is a common cause of respiratory disease in cattle, particularly calves. It is a negative-sense, single-stranded RNA virus that replicates in the cytoplasm of the cell. Similarly to other single-stranded RNA viruses, the genome of BRSV has a high mutation rate, which results in great antigenetic variation. Thus, BRSV can be split into four different subgroups based on antigen expression.