Stevens–Johnson syndrome (SJS) is a type of severe skin reaction. Together with toxic epidermal necrolysis (TEN) and Stevens–Johnson/toxic epidermal necrolysis (SJS/TEN), it forms a spectrum of disease, with SJS being less severe. Erythema multiforme (EM) is generally considered a separate condition. Early symptoms of SJS include fever and flu-like symptoms. A few days later, the skin begins to blister and peel, forming painful raw areas. Mucous membranes, such as the mouth, are also typically involved. Complications include dehydration, sepsis, pneumonia and multiple organ failure.

Pseudoephedrine (PSE) is a sympathomimetic drug of the phenethylamine and amphetamine chemical classes. It may be used as a nasal/sinus decongestant, as a stimulant, or as a wakefulness-promoting agent in higher doses.
Granuloma faciale is an uncommon benign chronic skin disease of unknown origin characterized by single or multiple cutaneous nodules, usually occurring over the face. Occasionally, extrafacial involvement is noted, most often on sun-exposed areas.
Photosensitivity is the amount to which an object reacts upon receiving photons, especially visible light. In medicine, the term is principally used for abnormal reactions of the skin, and two types are distinguished, photoallergy and phototoxicity. The photosensitive ganglion cells in the mammalian eye are a separate class of light-detecting cells from the photoreceptor cells that function in vision.
A maculopapular rash is a type of rash characterized by a flat, red area on the skin that is covered with small confluent bumps. It may only appear red in lighter-skinned people. The term "maculopapular" is a compound: macules are small, flat discolored spots on the surface of the skin; and papules are small, raised bumps. It is also described as erythematous, or red.

Cutaneous larva migrans is a skin disease in humans, caused by the larvae of various nematode parasites of the hookworm family (Ancylostomatidae). These parasites live in the intestines of dogs, cats, and wild animals and should not be confused with other members of the hookworm family for which humans are definitive hosts, namely Ancylostoma duodenale and Necator americanus.

Polymorphous light eruption (PLE), sometimes also called polymorphic light eruption (PMLE), is a non-life-threatening and potentially distressing skin condition that is triggered by sunlight and artificial UV exposure in a genetically susceptible person, particularly in temperate climates during the spring and early summer. Due to its many clinical appearances, it is named polymorphic or polymorphous and the terms are used interchangeably. The resulting itch can cause significant suffering.

Chemotherapy-induced acral erythema, also known as palmar-plantar erythrodesia or hand-foot syndrome is reddening, swelling, numbness and desquamation on palms of the hands and soles of the feet that can occur after chemotherapy in patients with cancer. Hand-foot syndrome is also rarely seen in sickle-cell disease. These skin changes usually are well demarcated. Acral erythema typically disappears within a few weeks after discontinuation of the offending drug.
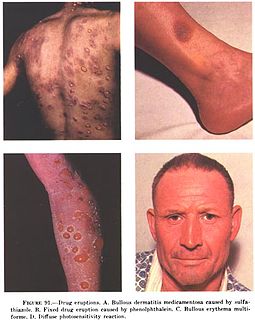
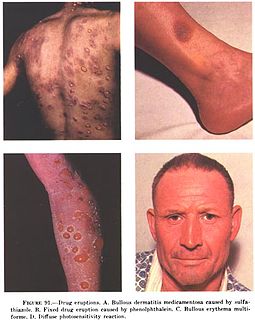
In medicine, a drug eruption is an adverse drug reaction of the skin. Most drug-induced cutaneous reactions are mild and disappear when the offending drug is withdrawn. These are called "simple" drug eruptions. However, more serious drug eruptions may be associated with organ injury such as liver or kidney damage and are categorized as "complex". Drugs can also cause hair and nail changes, affect the mucous membranes, or cause itching without outward skin changes.
Melanonychia is a black or brown pigmentation of the normal nail plate, and may be present as a normal finding on many digits in Afro-Caribbeans, as a result of trauma, systemic disease, or medications, or as a postinflammatory event from such localized events as lichen planus or fixed drug eruption.
Neutrophilic eccrine hidradenitis (NEH) usually is a cutaneous complication of chemotherapy, but it can also occur for other reasons. It consists of fever and non specific skin lesions. It is rare, and self-limited.
Anticonvulsant/sulfonamide hypersensitivity syndrome is a potentially serious hypersensitivity reaction that can be seen with medications with an aromatic amine chemical structure, such as aromatic anticonvulsants, sulfonamides, or other medications with an aromatic amine. Cross-reactivity should not occur between medications with an aromatic amine and medications without an aromatic amine ; therefore, these medications can be safely used in the future.
Photosensitive drug reaction secondary to medications may cause phototoxic, photoallergic, and lichenoid reactions, and photodistributed telangiectasias, as well as pseudoporphyria.

Acute generalized exanthematous pustulosis (AGEP) is a rare skin reaction that in 90% of cases is related to medication administration.
Bullous drug reaction most commonly refers to a drug reaction in the erythema multiforme group. These are uncommon reactions to medications, with an incidence of 0.4 to 1.2 per million person-years for toxic epidermal necrolysis and 1.2 to 6.0 per million person-years for Stevens–Johnson syndrome. The primary skin lesions are large erythemas, most often irregularly distributed and of a characteristic purplish-livid color, at times with flaccid blisters.
HIV disease-related drug reactions present in HIV-infected patients, especially those with helper T-cell counts between 25 and 200, immunosuppression that increases the risk for the development of adverse reactions to medications.

Iododermas are caused by iodides, with the most common sources of exposure being oral and intravenous contrast materials used to treat thyroid disease. The most common type of eruption is an acneiform eruption with numerous acutely inflamed follicular pustules, each surrounded by a ring of hyperemia.
Drug-induced pruritus is itchiness of the skin caused by medication, a pruritic reaction that is generalized.
Halogenodermas are skin eruptions that result after exposure to halogen-containing drugs or substances. This may last several weeks after drug use is discontinued. This is because of the slow elimination rate of iodides and bromides. Fluoroderma is a particular type of halogenoderma which is caused by fluoride. Fluoride is present in oral hygiene products such as toothpastes and mouth washes, hence this type of acne is seen mostly around the mouth and jawline. Acute fluoroderma has been observed in patients exposed to anaesthetics containing fluoride such as sevoflurane.