Allergies, also known as allergic diseases, are various conditions caused by hypersensitivity of the immune system to typically harmless substances in the environment. These diseases include hay fever, food allergies, atopic dermatitis, allergic asthma, and anaphylaxis. Symptoms may include red eyes, an itchy rash, sneezing, coughing, a runny nose, shortness of breath, or swelling. Note that food intolerances and food poisoning are separate conditions.
An allergen is a type of antigen that produces an abnormally vigorous immune response in which the immune system fights off a perceived threat that would otherwise be harmless to the body. Such reactions are called allergies.

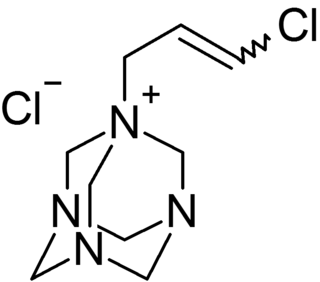
Methylisothiazolinone, MIT, or MI, is the organic compound with the formula S(CH)2C(O)NCH3. It is a white solid. Isothiazolinones, a class of heterocycles, are used as biocides in numerous personal care products and other industrial applications. MIT and related compounds have attracted much attention for their allergenic properties, e.g. contact dermatitis.

A food allergy is an abnormal immune response to food. The symptoms of the allergic reaction may range from mild to severe. They may include itchiness, swelling of the tongue, vomiting, diarrhea, hives, trouble breathing, or low blood pressure. This typically occurs within minutes to several hours of exposure. When the symptoms are severe, it is known as anaphylaxis. A food intolerance and food poisoning are separate conditions, not due to an immune response.

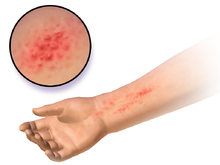
Contact dermatitis is a type of acute or chronic inflammation of the skin caused by exposure to chemical or physical agents. Symptoms of contact dermatitis can include itchy or dry skin, a red rash, bumps, blisters, or swelling. These rashes are not contagious or life-threatening, but can be very uncomfortable.

Latex allergy is a medical term encompassing a range of allergic reactions to the proteins present in natural rubber latex. It generally develops after repeated exposure to products containing natural rubber latex. When latex-containing medical devices or supplies come in contact with mucous membranes, the membranes may absorb latex proteins. In some susceptible people, the immune system produces antibodies that react immunologically with these antigenic proteins. Many items contain or are made from natural rubber, including shoe soles, pen grips, hot water bottles, elastic bands, rubber gloves, condoms, baby-bottle nipples, and balloons; consequently, there are many possible routes of exposure that may trigger a reaction. People with latex allergies may also have or develop allergic reactions to some fruits, such as bananas.
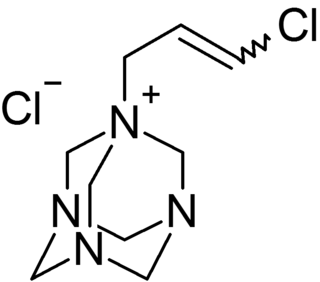
Quaternium-15 is a quaternary ammonium salt that has been used as a surfactant and preservative. It acts as an antimicrobial agent because it slowly releases formaldehyde, which is a preservative with biocidal properties.

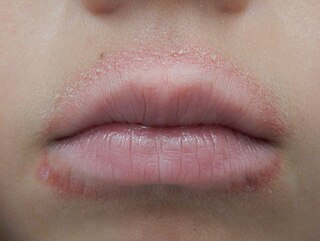
Stomatitis is inflammation of the mouth and lips. It refers to any inflammatory process affecting the mucous membranes of the mouth and lips, with or without oral ulceration.

A patch test is a diagnostic method used to determine which specific substances cause allergic inflammation of a patient's skin.

Soy allergy is a type of food allergy. It is a hypersensitivity to ingesting compounds in soy, causing an overreaction of the immune system, typically with physical symptoms, such as gastrointestinal discomfort, respiratory distress, or a skin reaction. Soy is among the eight most common foods inducing allergic reactions in children and adults. It has a prevalence of about 0.3% in the general population.

Allergic contact dermatitis (ACD) is a form of contact dermatitis that is the manifestation of an allergic response caused by contact with a substance; the other type being irritant contact dermatitis (ICD).

Balsam of Peru or Peru balsam, also known and marketed by many other names, is a balsam derived from a tree known as Myroxylon balsamum var. pereirae; it is found in El Salvador, where it is an endemic species.

Isothiazolinone (; sometimes isothiazolone) is an organic compound with the formula (CH)2SN(H)CO. A white solid, it is structurally related to isothiazole. Isothiazolone itself is of limited interest, but several of its derivatives are widely used preservatives and antimicrobials.
MELISA is a blood test that detects type IV hypersensitivity to metals, chemicals, environmental toxins and molds. Type IV hypersensitivity reactions, particularly to nickel, are well established and may affect 20% of the population.
Dogs are susceptible to allergies much like their human companions. Most allergies occur in dogs over 6 months old. A dog that is repeatedly exposed to a particular allergen becomes sensitized to it, and the immune system overreacts to a subsequent exposure, most commonly manifesting in the form of skin irritation. Some of the signs are redness, itching, hair loss, and recurring skin infections from the irritation. The dog may be more prone to scratching and licking at the irritated site, further exacerbating the problem.
Perfume intolerance or perfume allergy is a condition wherein people exhibit sensitivity or allergic reactions to ingredients in some perfumes and some other fragrances. It is a form of multiple chemical sensitivity, a more general phenomenon for this diagnosis.

Iodopropynyl Butyl Carbamate (IPBC) is a water-soluble preservative used globally in the paints & coatings, wood preservatives, personal care, and cosmetics industries. IPBC is a member of the carbamate family of biocides. IPBC was invented in the 1970s and has a long history of effective use as an antifungal technology.

The Nickel Directive was a European Union directive regulating the use of nickel in jewellery and other products that come into contact with the skin. Since 1 June 2009, it has been subsumed into the REACH Regulation, specifically item 27 of Annex XVII to that regulation. Nevertheless, the term Nickel Directive is still used to refer to the restrictions on nickel usage and the prescribed test method for quantifying nickel release from products EN 1811.

Nickel allergy is any of several allergic conditions provoked by exposure to the chemical element nickel. Nickel allergy often takes the form of nickel allergic contact dermatitis (Ni-ACD), a form of allergic contact dermatitis (ACD). Ni-ACD typically causes a rash that is red and itchy and that may be bumpy or scaly. The main treatment for it is avoiding contact with nickel-releasing metals, such as inexpensive jewelry. Another form of nickel allergy is a systemic form: systemic nickel allergy syndrome (SNAS) can mimic some of the symptoms of irritable bowel syndrome (IBS) and also has a dermatologic component.
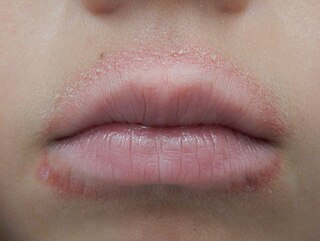
Lip licker's dermatitis is a type of skin inflammation around the lips due to damage by saliva from repetitive lip licking and is classified as a subtype of irritant contact cheilitis. The resulting scaling, redness, chapping, and crusting makes a well-defined ring around the lips. The rash may extend as far as the tongue can reach and usually does not occur at the corners of the mouth. It commonly occurs during winter months but some people can have it year-round if lip licking is a chronic habit.