Related Research Articles

Nummular dermatitis is one of the many forms of dermatitis. It is characterized by round or oval-shaped itchy lesions. The name comes from the Latin word "nummus," which means "coin."
Pseudopelade of Brocq is a flesh- to pink-colored, irregularly shaped alopecia that may begin in a moth-eaten pattern with eventual coalescence into larger patches of alopecia.
Unilateral nevoid telangiectasia presents with fine thread veins, typically over a segment of skin supplied by a particular nerve on one side of the body. It most frequently involves the trigeminal, C3 and C4, or nearby areas. The condition was named in 1970 by Victor Selmanowitz.

A tufted angioma, also known as an acquired tufted angioma, angioblastoma, angioblastoma of Nakagawa, hypertrophic hemangioma, progressive capillary hemangioma, and tufted hemangioma usually develops in infancy or early childhood on the neck and upper trunk, and is an ill-defined, dull red macule with a mottled appearance, varying from 2 to 5 cm in diameter.

Nevus lipomatosus superficialis is characterized by soft, yellowish papules or cerebriform plaques, usually of the buttock or thigh, less often of the ear or scalp, with a wrinkled rather than warty surface. It is usually congenital in origin or appears within the first three decades.
Glomeruloid hemangioma is a distinctive vascular tumor first described in 1990 when found to be associated with POEMS syndrome and Castleman disease. Glomeruloid hemangiomas can manifest as wine-red sessile or pedunculated papules, papulonodules, subcutaneous bluish compressible tumors, or small, firm, reddish-violaceous, dome-shaped papules.

Solitary mastocytoma, also known as cutaneous mastocytoma, may be present at birth or may develop during the first weeks of life, originating as a brown macule that urticates on stroking. Solitary mastocytoma is a round, erythematous, indurated lesion measuring 1-5 cm in diameter. It can be mildly itchy or asymptomatic and develops over time. Predilection is the head and neck, followed by the trunk, extremities, and flexural areas.
Cutaneous meningioma, also known as heterotopic meningeal tissue, and rudimentary meningocele is a developmental defect, and results from the presence of meningocytes outside the calvarium.
A cutaneous myxoma, or superficial angiomyxoma, consists of a multilobulated myxoid mass containing stellate or spindled fibroblasts with pools of mucin forming cleft-like spaces. There is often a proliferation of blood vessels and an inflammatory infiltrate. Staining is positive for vimentin, negative for cytokeratin and desmin, and variable for CD34, Factor VIIIa, SMA, MSA and S-100.
Erosive pustular dermatitis of the scalp presents with pustules, erosions, and crusts on the scalp of primarily older Caucasian females, and on biopsy, has a lymphoplasmacytic infiltrate with or without foreign body giant cells and pilosebaceous atrophy.
Recurrent palmoplantar hidradenitis, also known as idiopathic palmoplantar hidradenitis, idiopathic plantar hidradenitis, painful plantar erythema, palmoplantar eccrine hidradenitis, and plantar panniculitis, is primarily a disorder of healthy children and young adults, characterized by lesions that are primarily painful, subcutaneous nodules on the plantar surface, resembling erythema nodosum.
Erythromelanosis follicularis faciei et colli is an erythematous pigmentary disease involving the follicles, characterized by a reddish-brown, sharply demarcated, symmetrical discoloration involving the preauricular and maxillary regions.

Linear IgA bullous dermatosis is a rare immune-mediated blistering skin disease frequently associated with medication exposure, especially vancomycin, with men and women being equally affected. It was first described by Tadeusz Chorzelski in 1979 and may be divided into two types:
Multiple minute digitate hyperkeratosis, also known as digitate keratoses, disseminated spiked hyperkeratosis, familial disseminated piliform hyperkeratosis, and minute aggregate keratosis is a rare cutaneous condition, with about half of cases being familial, inherited in an autosomal dominant fashion, while the other half are sporadic.
Reticular erythematous mucinosis (REM) is a skin condition caused by fibroblasts producing abnormally large amounts of mucopolysaccharides. It is a disease that tends to affect women in the third and fourth decades of life.
Parakeratosis pustulosa is a cutaneous condition which is exclusively seen in children, usually involving one finger, most commonly the thumb or index finger, with the affected nail showing subungual hyperkeratosis and onycholysis.
Annular elastolytic giant-cell granuloma is a cutaneous condition characterized histologically by a dermal infiltrate of macrophages.
Nevoid hypertrichosis is a cutaneous condition characterized by the growth of terminal hairs in a circumscribed area. Nevoid hypertrichosis often presents shortly after birth. The cause of nevoid hypertrichosis is unknown. The diagnosis is made based of clinical and histopathological examination.
Multinucleate cell angiohistiocytoma (MCAH) is a cutaneous condition that presents as slowly growing, multiple, discrete but grouped, red to violaceous papules
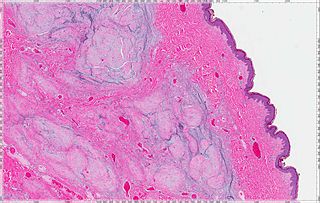
Histopathology of dermatitis can be performed in uncertain cases of inflammatory skin condition that remain uncertain after history and physical examination.
References
- 1 2 Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 978-1-4160-2999-1.
- ↑ "Munks Roll Details for Peter Edward Darrell Sheldon Wilkinson". munksroll.rcplondon.ac.uk. Retrieved 2017-11-10.
- 1 2 Griffiths, Christopher E. M.; Bleiker, Tanya O.; Creamer, Daniel; Ingram, John R.; Simpson, Rosalind C. (2022). "14. Eczematous disorders". Rook's Dermatology Handbook. John Wiley & Sons. p. 211. ISBN 978-1-119-42819-0.
- 1 2 3 Kalia, Sunil; Adams, Stewart P. (2005-09-09). "Dry, red, shinny lesions on the feet". Canadian Family Physician. 51 (9). College of Family Physicians of Canada: 1203, 1213. PMC 1479460 . PMID 16190171.
- 1 2 Kumar, HariKishan; Naveen, S; Shankar, Keerthi (2016). "Juvenile plantar dermatosis: A barrier disease beyond eczema: An open prospective uncontrolled study in a tertiary care hospital of South India". Indian Journal of Paediatric Dermatology. 17 (1). Medknow: 13. doi: 10.4103/2319-7250.173158 . ISSN 2319-7250.
- ↑ Shenoi, SD; Balachandran, C; Mehta, VandanaRai; Brar, KamalJeet (2005). "Clinical profile of forefoot eczema: A study of 42 cases". Indian Journal of Dermatology, Venereology and Leprology. 71 (3). Scientific Scholar: 179–181. doi: 10.4103/0378-6323.16233 . ISSN 0378-6323. PMID 16394407.