Dermatitis is inflammation of the skin, typically characterized by itchiness, redness and a rash. In cases of short duration, there may be small blisters, while in long-term cases the skin may become thickened. The area of skin involved can vary from small to covering the entire body. Dermatitis is often called eczema, and the difference between those terms is not standardized.

Vitiligo is a disorder that causes the skin to lose its color. Specific causes are unknown but studies suggest a link to immune system changes.

Tinea versicolor is a condition characterized by a skin eruption on the trunk and proximal extremities. The majority of tinea versicolor is caused by the fungus Malassezia globosa, although Malassezia furfur is responsible for a small number of cases. These yeasts are normally found on the human skin and become troublesome only under certain circumstances, such as a warm and humid environment, although the exact conditions that cause initiation of the disease process are poorly understood.

Irritant diaper dermatitis is a generic term applied to skin rash in the diaper nappy area that are caused by various skin disorders and/or irritants.

Ichthyosis is a family of genetic skin disorders characterized by dry, thickened, scaly skin. The more than 20 types of ichthyosis range in severity of symptoms, outward appearance, underlying genetic cause and mode of inheritance. Ichthyosis comes from the Greek ἰχθύς ichthys, literally "fish", since dry, scaly skin is the defining feature of all forms of ichthyosis.

Contact dermatitis is a type of acute or chronic inflammation of the skin caused by exposure to chemical or physical agents. Symptoms of contact dermatitis can include itchy or dry skin, a red rash, bumps, blisters, or swelling. These rashes are not contagious or life-threatening, but can be very uncomfortable.

Lichen planus (LP) is a chronic inflammatory and immune-mediated disease that affects the skin, nails, hair, and mucous membranes. It is not an actual lichen, and is only named that because it looks like one. It is characterized by polygonal, flat-topped, violaceous papules and plaques with overlying, reticulated, fine white scale, commonly affecting dorsal hands, flexural wrists and forearms, trunk, anterior lower legs and oral mucosa. The hue may be gray-brown in people with darker skin. Although there is a broad clinical range of LP manifestations, the skin and oral cavity remain as the major sites of involvement. The cause is unknown, but it is thought to be the result of an autoimmune process with an unknown initial trigger. There is no cure, but many different medications and procedures have been used in efforts to control the symptoms.

Hypopigmentation is characterized specifically as an area of skin becoming lighter than the baseline skin color, but not completely devoid of pigment. This is not to be confused with depigmentation, which is characterized as the absence of all pigment. It is caused by melanocyte or melanin depletion, or a decrease in the amino acid tyrosine, which is used by melanocytes to make melanin. Some common genetic causes include mutations in the tyrosinase gene or OCA2 gene. As melanin pigments tend to be in the skin, eye, and hair, these are the commonly affected areas in those with hypopigmentation.

Pityriasis rosea is a type of skin rash. Classically, it begins with a single red and slightly scaly area known as a "herald patch". This is then followed, days to weeks later, by an eruption of many smaller scaly spots; pinkish with a red edge in people with light skin and greyish in darker skin. About 20% of cases show atypical deviations from this pattern. It usually lasts less than three months and goes away without treatment. Sometimes malaise or a fever may occur before the start of the rash or itchiness, but often there are few other symptoms.

Lichen sclerosus (LS) is a chronic, inflammatory skin disease of unknown cause which can affect any body part of any person but has a strong preference for the genitals and is also known as balanitis xerotica obliterans (BXO) when it affects the penis. Lichen sclerosus is not contagious. There is a well-documented increase of skin cancer risk in LS, potentially improvable with treatment. LS in adult age women is normally incurable, but improvable with treatment, and often gets progressively worse if not treated properly. Most males with mild or intermediate disease restricted to prepuce or glans can be cured by either medical or surgical treatment.

Nummular dermatitis is one of the many forms of dermatitis. it is characterized by round or oval-shaped itchy lesions. The name comes from the Latin word "nummus," which means "coin."

Atopic dermatitis (AD), also known as atopic eczema, is a long-term type of inflammation of the skin (dermatitis). It results in itchy, red, swollen, and cracked skin. Clear fluid may come from the affected areas, which often thickens over time. While the condition may occur at any age, it typically starts in childhood, with changing severity over the years. In children under one year of age, much of the body may be affected. As children get older, the areas on the insides of the knees and elbows are most commonly affected. In adults, the hands and feet are most commonly affected. Scratching the affected areas worsens the symptoms, and those affected have an increased risk of skin infections. Many people with atopic dermatitis develop hay fever or asthma.

Cholinergic urticaria (CU) presents with tiny very itchy wheals and small bumps on a reddish background.

Hand eczema presents on the palms and soles, and may sometimes be difficult or impossible to differentiate from atopic dermatitis, allergic contact dermatitis, and psoriasis, which also commonly involve the hands. Even a biopsy of all these conditions may not result in a definitive diagnosis, as all three conditions may demonstrate spongiosis and crusting on the hands.

Guttate psoriasis is a type of psoriasis that presents as small lesions over the upper trunk and proximal extremities; it is found frequently in young adults.
Malassezia sympodialis is a species in the genus Malassezia. It is characterized by a pronounced lipophily, unilateral, percurrent or sympodial budding and an irregular, corrugated cell wall ultrastructure. It is one of the most common species found on the skin of healthy and diseased individuals. It is considered to be part of the skin's normal human microbiota and begins to colonize the skin of humans shortly after birth. Malassezia sympodialis, often has a symbiotic or commensal relationship with its host, but it can act as a pathogen causing a number of different skin diseases, such as atopic dermatitis.

Nickel allergy or nickel allergic contact dermatitis (Ni-ACD) is a form of allergic contact dermatitis (ACD) caused by exposure to the chemical element nickel. It typically causes a rash that is red and itchy and that may be bumpy or scaly. The main treatment is avoiding contact with nickel-releasing metals, such as wearing inexpensive jewelry.
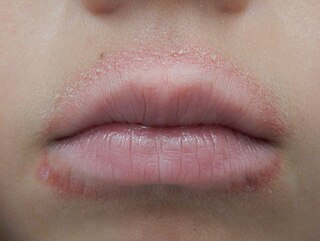
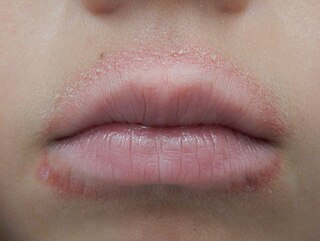
Lip licker's dermatitis is a type of skin inflammation around the lips due to damage by saliva from repetitive lip licking and is classified as a subtype of irritant contact cheilitis. The resulting scaling, redness, chapping, and crusting makes a well-defined ring around the lips. The rash may extend as far as the tongue can reach and usually does not occur at the corners of the mouth. It commonly occurs during winter months but some people can have it year-round if lip licking is a chronic habit.

Topical glucocorticoids are the topical forms of glucocorticoids. Topical glucocorticoids are used in the treatment of many skin conditions. They provide anti-inflammatory, antimitotic, and immune-system suppressing actions through various mechanisms.