Related Research Articles

Vitiligo is a chronic autoimmune disorder that causes patches of skin to lose pigment or color. The cause of vitiligo is unknown, but it may be related to immune system changes, genetic factors, stress, or sun exposure. Treatment options include topical medications, light therapy, surgery and cosmetics. The condition can show up on any skin type as a light peachy color and can appear on any place on the body in all sizes. The spots on the skin known as vitiligo are also able to “change” as spots lose and regain pigment; they will stay in relatively the same areas but can move over time and some big patches can move through the years but never disappear overnight.

Tinea versicolor is a condition characterized by a skin eruption on the trunk and proximal extremities. The majority of tinea versicolor is caused by the fungus Malassezia globosa, although Malassezia furfur is responsible for a small number of cases. These yeasts are normally found on the human skin and become troublesome only under certain conditions, such as a warm and humid environment, although the exact conditions that cause initiation of the disease process are poorly understood.

Hyperpigmentation is the darkening of an area of skin or nails caused by increased melanin.

Hypopigmentation is characterized specifically as an area of skin becoming lighter than the baseline skin color, but not completely devoid of pigment. This is not to be confused with depigmentation, which is characterized as the absence of all pigment. It is caused by melanocyte or melanin depletion, or a decrease in the amino acid tyrosine, which is used by melanocytes to make melanin. Some common genetic causes include mutations in the tyrosinase gene or OCA2 gene. As melanin pigments tend to be in the skin, eye, and hair, these are the commonly affected areas in those with hypopigmentation.

Melasma is a tan or dark skin discoloration. Melasma is thought to be caused by sun exposure, genetic predisposition, hormone changes, and skin irritation. Although it can affect anyone, it is particularly common in women, especially pregnant women and those who are taking oral or patch contraceptives or hormone replacement therapy medications.

A lentigo is a small pigmented spot on the skin with a clearly defined edge, surrounded by normal-appearing skin. It is a harmless (benign) hyperplasia of melanocytes which is linear in its spread. This means the hyperplasia of melanocytes is restricted to the cell layer directly above the basement membrane of the epidermis where melanocytes normally reside. This is in contrast to the "nests" of multi-layer melanocytes found in moles. Because of this characteristic feature, the adjective "lentiginous" is used to describe other skin lesions that similarly proliferate linearly within the basal cell layer.

Pityriasis lichenoides represents a distinct subset of inflammatory skin disorders that includes pityriasis lichenoides chronica, febrile ulceronecrotic Mucha-Habermann disease, and pityriasis lichenoides et varioliformis acuta (PLEVA).
Pityriasis alba is a skin condition, a type of dermatitis, commonly seen in children and young adults as dry, fine-scaled, pale patches on the face. It is self-limiting and usually only requires use of moisturizer creams.
Pigmentation disorders are disturbances of human skin color. There may be a loss or reduction, which may be related to loss of melanocytes or the inability of melanocytes to produce melanin or transport melanosomes correctly.
Halo nevus is a mole that is surrounded by a pale ring or 'halo'. It is generally noticed in the summer, when surrounding skin tans, and usually occurs on the chest, but can be anywhere. There may be one or more typically several. Onset is usually in teenagers and young adults. It typically follows a pattern of appearing at first as a dark mole surrounded by a halo before the nevus fades and disappears. A single halo nevus like lesion appearing in an older adult may be a melanoma.

Poliosis circumscripta, commonly referred to as a "white forelock", is a condition characterized by localized patches of white hair due to a reduction or absence of melanin in hair follicles. Although traditionally associated with the scalp, poliosis can affect any hairy area on the body, including eyebrows, eyelashes, and beards. Microscopically, poliosis is marked by the lack of melanin or melanocytes in the hair bulbs, though epidermal melanocytes typically remain unaffected unless associated with conditions like vitiligo.
Interstitial granulomatous dermatitis with arthritis (IGDA) or Ackerman dermatitis syndrome is a skin condition that most commonly presents with symmetrical round-to-oval red or violet plaques on the flanks, armpits, inner thighs, and lower abdomen.
Erosive pustular dermatitis of the scalp presents with pustules, erosions, and crusts on the scalp of primarily older Caucasian females, and on biopsy, has a lymphoplasmacytic infiltrate with or without foreign body giant cells and pilosebaceous atrophy.

Airbag dermatitis is skin irritation secondary to the deployment of airbags. The diagnosis of "air bag dermatitis" is relatively recent; the first case was reported in 1994.

Nevus depigmentosus is a loss of pigment in the skin which can be easily differentiated from vitiligo. Although age factor has not much involvement in the nevus depigmentosus but in about 19% of the cases these are noted at birth. Their size may however grow in proportion to growth of the body. The distribution is also fairly stable and are nonprogressive hypopigmented patches. The exact cause of nevus depigmentosus is still not clearly understood. A sporadic defect in the embryonic development has been suggested to be a causative factor. It has been described as "localised albinism", though this is incorrect.
Rheumatoid neutrophilic dermatitis, also known as rheumatoid neutrophilic dermatosis, is a cutaneous condition associated with rheumatoid arthritis.

Rhododendrol (RD) also called 4-[(3R)-3-hydroxybutyl]phenol (systemic name), is an organic compound with the formula C10H14O2. It is a naturally occurring ingredient present in many plants, such as the Rhododendron. The phenolic compound was first developed in 2010 as a tyrosinase inhibitor for skin-lightening cosmetics. In 2013, after rhododendrol reportedly caused skin depigmentation in consumers using RD-containing skin-brightening cosmetics, the cosmetics were withdrawn from the market. The skin condition, caused by RD, is called RD-induced leukoderma. Rhododendrol exerts melanocyte cytotoxicity via a tyrosinase-dependent mechanism. It has been shown to impair the normal proliferation of melanocytes through reactive oxygen species-dependent activation of GADD45. It is now well established that rhododendrol is a potent tyrosinase inhibitor.
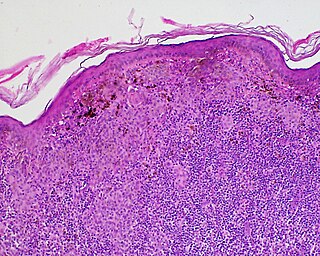
Histopathology of dermatitis can be performed in uncertain cases of inflammatory skin condition that remain uncertain after history and physical examination.
Postinflammatory hyperpigmentation (PIH) is a skin condition characterized by the darkening of the skin (hyperpigmentation) following an inflammatory injury, such as acne, dermatitis, infectious disease, or trauma. Less frequently, it may occur as a complication of a medical procedure performed on the skin. It is a common cause of skin discoloration and can affect individuals of all skin types.
References
- ↑ Marks, James G; Miller, Jeffery (2006). Lookingbill and Marks' Principles of Dermatology (4th ed.). Elsevier Inc. ISBN 1-4160-3185-5.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Vachiramon, V.; Thadanipon, K. (2011). "Postinflammatory hypopigmentation: Postinflammatory hypopigmentation". Clinical and Experimental Dermatology. 36 (7): 708–714. doi:10.1111/j.1365-2230.2011.04088.x. PMID 21671990. S2CID 28162346.
- ↑ Larrègue, M; Martin, J; Bressieux, J M; Canuel, C; De Giacomoni, P; Ramdenée, P; Babin, P (1985). "Vitiligoid achromias and severe atopic dermatitis. Apropos of 4 cases". Annales de dermatologie et de venereologie (in French). 112 (8): 589–600. PMID 4096464.
- ↑ Peramiquel, Laura; Baselga, Eulàlia; Dalmau, Joan; Roé, Esther; del Mar Campos, Maria; Alomar, Agustín (2006-01-13). "Lichen striatus: clinical and epidemiological review of 23 cases". European Journal of Pediatrics. 165 (4). Springer Science and Business Media LLC: 267–269. doi:10.1007/s00431-005-0032-9. ISSN 0340-6199. PMID 16411095. S2CID 36626542.
- ↑ Lane, Tanda N; Parker, Sareeta S (March 2010). "Pityriasis lichenoides chronica in black patients" (PDF). Cutis. 85 (3): 125–129. PMID 20408509 . Retrieved 1 March 2024.
- ↑ El-Bishry, M. Adly; Nassar, Alia M.; El-Maghraby, Magda Z. (1979). "Tattooing, A New Hope for Secondary Leukoderma". Scandinavian Journal of Plastic and Reconstructive Surgery. 13 (1). Informa UK Limited: 147–153. doi:10.3109/02844317909013044. ISSN 0036-5556. PMID 451462.
- ↑ Xiang, Wenzhong; Xu, Aie; Xu, Jin; Bi, Zhigang; Shang, Yingbin; Ren, Qiushi (2010-02-24). "In vivo confocal laser scanning microscopy of hypopigmented macules: a preliminary comparison of confocal images in vitiligo, nevus depigmentosus and postinflammatory hypopigmentation". Lasers in Medical Science. 25 (4). Springer Science and Business Media LLC: 551–558. doi:10.1007/s10103-010-0764-2. ISSN 0268-8921. PMID 20180143. S2CID 9185505.
- ↑ High, Whitney A.; Pandya, Amit G. (2006). "Pilot trial of 1% pimecrolimus cream in the treatment of seborrheic dermatitis in African American adults with associated hypopigmentation". Journal of the American Academy of Dermatology. 54 (6). Elsevier BV: 1083–1088. doi:10.1016/j.jaad.2006.01.011. ISSN 0190-9622. PMID 16713477.
- ↑ Ruiz-Maldonado, Ramon; de la Luz Orozco-Covarrubias, Maria (1997). "Postinflammatory hypopigmentation and hyperpigmentation". Seminars in Cutaneous Medicine and Surgery. 16 (1). Frontline Medical Communications, Inc.: 36–43. doi:10.1016/s1085-5629(97)80034-x. ISSN 1085-5629. PMID 9125764.
- ↑ Alexiades-Armenakas, Macrene R.; Bernstein, Leonard J.; Friedman, Paul M.; Geronemus, Roy G. (2004-08-01). "The Safety and Efficacy of the 308-nm Excimer Laser for Pigment Correction of Hypopigmented Scars and Striae Alba". Archives of Dermatology. 140 (8). American Medical Association (AMA): 955–960. doi:10.1001/archderm.140.8.955. ISSN 0003-987X. PMID 15313811.
- ↑ Suvanprakorn, Pichit; Dee-Ananlap, Sompong; Pongsomboon, Chalit; Klaus, Sidney N. (1985). "Melanocyte autologous grafting for treatment of leukoderma". Journal of the American Academy of Dermatology. 13 (6). Elsevier BV: 968–974. doi:10.1016/s0190-9622(85)70247-2. ISSN 0190-9622. PMID 3908515.
- ↑ FALABELLA, RAFAEL (1987). "Postdermabrasion Leukoderma". The Journal of Dermatologic Surgery and Oncology. 13 (1). Wiley: 44–48. doi:10.1111/j.1524-4725.1987.tb00495.x. ISSN 0148-0812. PMID 3540047.