The peripheral nervous system (PNS) is one of two components that make up the nervous system of bilateral animals, with the other part being the central nervous system (CNS). The PNS consists of the nerves and ganglia outside the brain and spinal cord. The main function of the PNS is to connect the CNS to the limbs and organs, essentially serving as a relay between the brain and spinal cord and the rest of the body. Unlike the CNS, the PNS is not protected by the vertebral column and skull, or by the blood–brain barrier, which leaves it exposed to toxins and mechanical injuries.

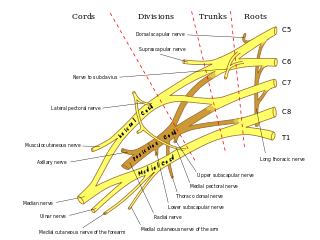
The brachial plexus is a network of nerves formed by the anterior rami of the lower four cervical nerves and first thoracic nerve. This plexus extends from the spinal cord, through the cervicoaxillary canal in the neck, over the first rib, and into the armpit. It supplies afferent and efferent nerve fibers to the chest, shoulder, arm, forearm, and hand.

The phrenic nerve is a mixed motor/sensory nerve which originates from the C3-C5 spinal nerves in the neck. The nerve is important for breathing because it provides exclusive motor control of the diaphragm, the primary muscle of respiration. In humans, the right and left phrenic nerves are primarily supplied by the C4 spinal nerve, but there is also contribution from the C3 and C5 spinal nerves. From its origin in the neck, the nerve travels downward into the chest to pass between the heart and lungs towards the diaphragm.

A Pancoast tumor is a tumor of the apex of the lung. It is a type of lung cancer defined primarily by its location situated at the top end of either the right or left lung. It typically spreads to nearby tissues such as the ribs and vertebrae. Most Pancoast tumors are non-small-cell lung cancers.
Neurotmesis is part of Seddon's classification scheme used to classify nerve damage. It is the most serious nerve injury in the scheme. In this type of injury, both the nerve and the nerve sheath are disrupted. While partial recovery may occur, complete recovery is impossible.
Axonotmesis is an injury to the peripheral nerve of one of the extremities of the body. The axons and their myelin sheath are damaged in this kind of injury, but the endoneurium, perineurium and epineurium remain intact. Motor and sensory functions distal to the point of injury are completely lost over time leading to Wallerian degeneration due to ischemia, or loss of blood supply. Axonotmesis is usually the result of a more severe crush or contusion than neurapraxia.

The suprascapular nerve is a nerve that branches from the upper trunk of the brachial plexus. It is responsible for the innervation of two of the muscles that originate from the scapula, namely the supraspinatus and infraspinatus muscles.
In medicine, a stinger, also called a burner or nerve pinch injury, is a neurological injury suffered by athletes, mostly in high-contact sports such as ice hockey, rugby, American football, and wrestling. The spine injury is characterized by a shooting or stinging pain that travels down one arm, followed by numbness and weakness in the parts of the arms, including the biceps, deltoid, and spinati muscles. Many athletes in contact sports have suffered stingers, but they are often unreported to medical professionals.

Neuritis is inflammation of a nerve or the general inflammation of the peripheral nervous system. Inflammation, and frequently concomitant demyelination, cause impaired transmission of neural signals and leads to aberrant nerve function. Neuritis is often conflated with neuropathy, a broad term describing any disease process which affects the peripheral nervous system. However, neuropathies may be due to either inflammatory or non-inflammatory causes, and the term encompasses any form of damage, degeneration, or dysfunction, while neuritis refers specifically to the inflammatory process.

The scalene muscles are a group of three pairs of muscles in the lateral neck, namely the anterior scalene, middle scalene, and posterior scalene. They are innervated by the third to the eight cervical spinal nerves (C3-C8).

A brachial plexus injury (BPI), also known as brachial plexus lesion, is an injury to the brachial plexus, the network of nerves that conducts signals from the spinal cord to the shoulder, arm and hand. These nerves originate in the fifth, sixth, seventh and eighth cervical (C5–C8), and first thoracic (T1) spinal nerves, and innervate the muscles and skin of the chest, shoulder, arm and hand.

A neuromuscular disease is any disease affecting the peripheral nervous system (PNS), the neuromuscular junction, or skeletal muscle, all of which are components of the motor unit. Damage to any of these structures can cause muscle atrophy and weakness. Issues with sensation can also occur.
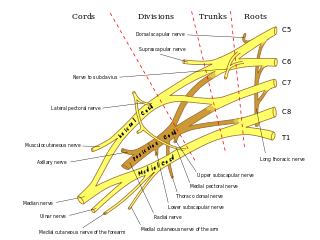
The subclavian nerve, also known as the nerve to the subclavius, is small branch of the upper trunk of the brachial plexus. It contains axons from C5 and C6. The subclavian nerve innervates the subclavius muscle.

Parsonage–Turner syndrome, also known as acute brachial neuropathy and neuralgic amyotrophy and abbreviated PTS, is a syndrome of unknown cause; although many specific risk factors have been identified, the cause is still unknown. The condition manifests as a rare set of symptoms most likely resulting from autoimmune inflammation of unknown cause of the brachial plexus.

The ventral ramus is the anterior division of a spinal nerve. The ventral rami supply the antero-lateral parts of the trunk and the limbs. They are mainly larger than the dorsal rami.
Critical illness polyneuropathy (CIP) and critical illness myopathy (CIM) are overlapping syndromes of diffuse, symmetric, flaccid muscle weakness occurring in critically ill patients and involving all extremities and the diaphragm with relative sparing of the cranial nerves. CIP and CIM have similar symptoms and presentations and are often distinguished largely on the basis of specialized electrophysiologic testing or muscle and nerve biopsy. The causes of CIP and CIM are unknown, though they are thought to be a possible neurological manifestation of systemic inflammatory response syndrome. Corticosteroids and neuromuscular blocking agents, which are widely used in intensive care, may contribute to the development of CIP and CIM, as may elevations in blood sugar, which frequently occur in critically ill patients.
Plexopathy is a disorder of the network of nerves in the brachial or lumbosacral plexus. Symptoms include pain, muscle weakness, and sensory deficits (numbness).
Anterior interosseous syndrome is a medical condition in which damage to the anterior interosseous nerve (AIN), a distal motor and sensory branch of the median nerve, classically with severe weakness of the pincer movement of the thumb and index finger, and can cause transient pain in the wrist.

Brachial plexus block is a regional anesthesia technique that is sometimes employed as an alternative or as an adjunct to general anesthesia for surgery of the upper extremity. This technique involves the injection of local anesthetic agents in close proximity to the brachial plexus, temporarily blocking the sensation and ability to move the upper extremity. The subject can remain awake during the ensuing surgical procedure, or they can be sedated or even fully anesthetized if necessary.