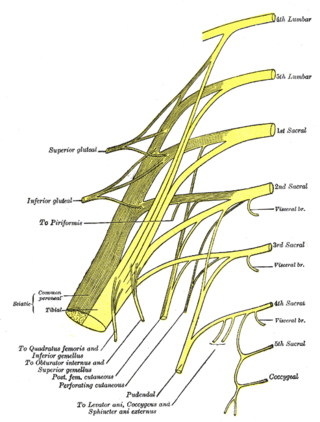
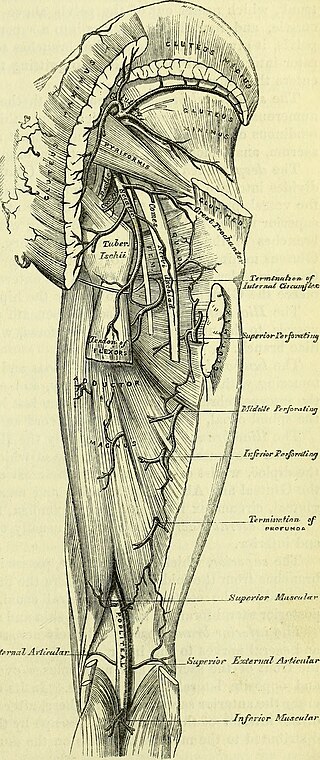
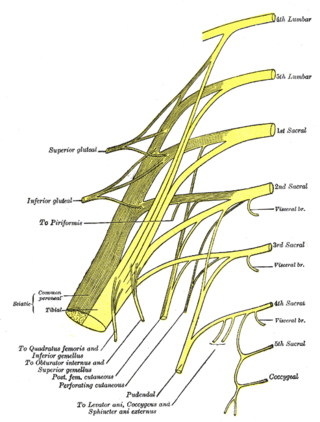
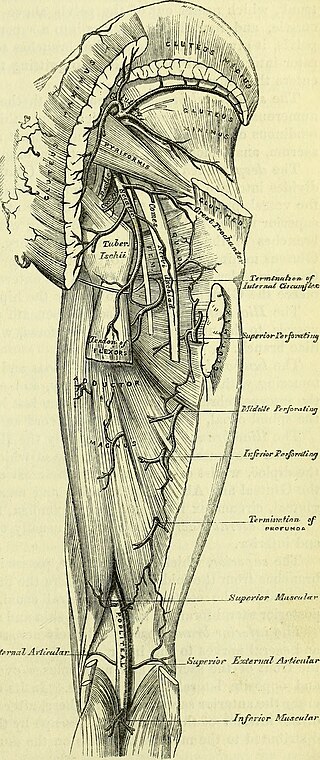
The sciatic nerve, also called the ischiadic nerve, is a large nerve in humans and other vertebrate animals. It is the largest branch of the sacral plexus and runs alongside the hip joint and down the lower limb. It is the longest and widest single nerve in the human body, going from the top of the leg to the foot on the posterior aspect. The sciatic nerve has no cutaneous branches for the thigh. This nerve provides the connection to the nervous system for the skin of the lateral leg and the whole foot, the muscles of the back of the thigh, and those of the leg and foot. It is derived from spinal nerves L4 to S3. It contains fibres from both the anterior and posterior divisions of the lumbosacral plexus.
Pudendal nerve entrapment (PNE), also known as Alcock canal syndrome, is an uncommon source of chronic pain in which the pudendal nerve is entrapped or compressed in Alcock's canal. There are several different types of PNE based on the site of entrapment anatomically. Pain is positional and is worsened by sitting. Other symptoms include genital numbness, fecal incontinence and urinary incontinence.
Diabetic neuropathy includes various types of nerve damage associated with diabetes mellitus. The most common form, diabetic peripheral neuropathy, affects 30% of all diabetic patients. Symptoms depend on the site of nerve damage and can include motor changes such as weakness; sensory symptoms such as numbness, tingling, or pain; or autonomic changes such as urinary symptoms. These changes are thought to result from a microvascular injury involving small blood vessels that supply nerves. Relatively common conditions which may be associated with diabetic neuropathy include distal symmetric polyneuropathy; third, fourth, or sixth cranial nerve palsy; mononeuropathy; mononeuropathy multiplex; diabetic amyotrophy; and autonomic neuropathy.

Peroneal nerve paralysis is a paralysis on common fibular nerve that affects patient’s ability to lift the foot at the ankle. The condition was named after Friedrich Albert von Zenker. Peroneal nerve paralysis usually leads to neuromuscular disorder, peroneal nerve injury, or foot drop which can be symptoms of more serious disorders such as nerve compression. The origin of peroneal nerve palsy has been reported to be associated with musculoskeletal injury or isolated nerve traction and compression. Also it has been reported to be mass lesions and metabolic syndromes. Peroneal nerve is most commonly interrupted at the knee and possibly at the joint of hip and ankle. Most studies reported that about 30% of peroneal nerve palsy is followed from knee dislocations.

Tinel's sign is a way to detect irritated nerves. It is performed by lightly tapping (percussing) over the nerve to elicit a sensation of tingling or "pins and needles" in the distribution of the nerve. Percussion is usually performed moving distal to proximal. It is named after Jules Tinel.
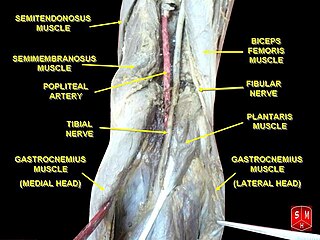
The tibial nerve is a branch of the sciatic nerve. The tibial nerve passes through the popliteal fossa to pass below the arch of soleus.
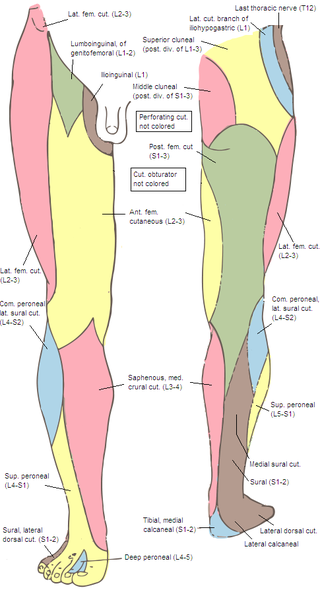
Meralgia paresthetica or meralgia paraesthetica is pain or abnormal sensations in the outer thigh not caused by injury to the thigh, but by injury to a nerve which provides sensation to the lateral thigh.

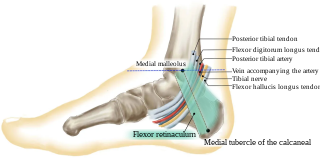
The flexor hallucis longus muscle (FHL) attaches to the plantar surface of phalanx of the great toe and is responsible for flexing that toe. The FHL is one of the three deep muscles of the posterior compartment of the leg, the others being the flexor digitorum longus and the tibialis posterior. The tibialis posterior is the most powerful of these deep muscles. All three muscles are innervated by the tibial nerve which comprises half of the sciatic nerve.

The flexor digitorum longus muscle is situated on the tibial side of the leg. At its origin it is thin and pointed, but it gradually increases in size as it descends. It serves to flex the second, third, fourth, and fifth toes.
The common fibular nerve is a nerve in the lower leg that provides sensation over the posterolateral part of the leg and the knee joint. It divides at the knee into two terminal branches: the superficial fibular nerve and deep fibular nerve, which innervate the muscles of the lateral and anterior compartments of the leg respectively. When the common fibular nerve is damaged or compressed, foot drop can ensue.
The flexor retinaculum of foot is a strong fibrous band in the foot.
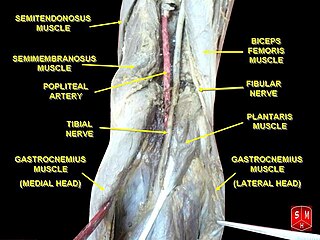
The popliteal artery entrapment syndrome (PAES) is an uncommon pathology that occurs when the popliteal artery is compressed by the surrounding popliteal fossa myofascial structures. This results in claudication and chronic leg ischemia. This condition mainly occurs more in young athletes than in the elderlies. Elderlies, who present with similar symptoms, are more likely to be diagnosed with peripheral artery disease with associated atherosclerosis. Patients with PAES mainly present with intermittent feet and calf pain associated with exercises and relieved with rest. PAES can be diagnosed with a combination of medical history, physical examination, and advanced imaging modalities such as duplex ultrasound, computer tomography, or magnetic resonance angiography. Management can range from non-intervention to open surgical decompression with a generally good prognosis. Complications of untreated PAES can include stenotic artery degeneration, complete popliteal artery occlusion, distal arterial thromboembolism, or even formation of an aneurysm.
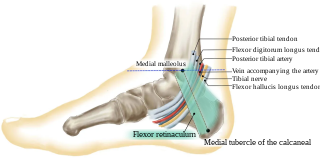
The tarsal tunnel is a passage found along the inner leg underneath the medial malleolus of the ankle.
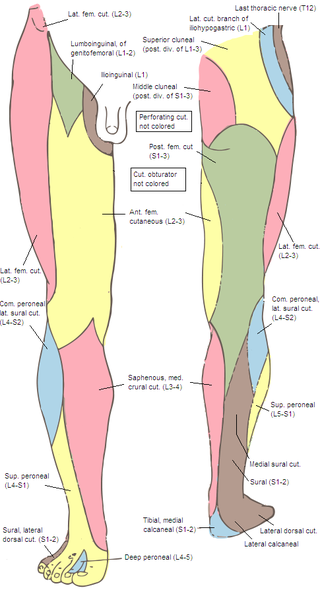
The superior cluneal nerves are pure sensory nerves that innervate the skin of the upper part of the buttocks. They are the terminal ends of the L1-L3 spinal nerve dorsal rami lateral branches. They are one of three different types of cluneal nerves. They travel inferiorly through multiple layers of muscles, then traverse osteofibrous tunnels between the thoracolumbar fascia and iliac crest.

Idiopathic ulnar neuropathy at the elbow is a condition where pressure on the ulnar nerve as it passes through the cubital tunnel causes ulnar neuropathy. The symptoms of neuropathy are paresthesia (tingling) and numbness primarily affecting the little finger and ring finger of the hand. Ulnar neuropathy can progress to weakness and atrophy of the muscles in the hand. Symptoms can be alleviated by the use of a splint to prevent the elbow from flexing while sleeping.

Ulnar neuropathy is a disorder involving the ulnar nerve. Ulnar neuropathy may be caused by entrapment of the ulnar nerve with resultant numbness and tingling. It may also cause weakness or paralysis of the muscles supplied by the nerve. Ulnar neuropathy may affect the elbow as cubital tunnel syndrome. At the wrist a similar neuropathy is ulnar tunnel syndrome.

Nerve compression syndrome, or compression neuropathy, or nerve entrapment syndrome, is a medical condition caused by chronic, direct pressure on a peripheral nerve. It is known colloquially as a trapped nerve, though this may also refer to nerve root compression. Its symptoms include pain, tingling, numbness and muscle weakness. The symptoms affect just one particular part of the body, depending on which nerve is affected. The diagnosis is largely clinical and can be confirmed with diagnostic nerve blocks. Occasionally imaging and electrophysiology studies aid in the diagnosis. Timely diagnosis is important as untreated chronic nerve compression may cause permanent damage. A surgical nerve decompression can relieve pressure on the nerve but cannot always reverse the physiological changes that occurred before treatment. Nerve injury by a single episode of physical trauma is in one sense an acute compression neuropathy but is not usually included under this heading, as chronic compression takes a unique pathophysiological course.

Injuries to the arm, forearm or wrist area can lead to various nerve disorders. One such disorder is median nerve palsy. The median nerve controls the majority of the muscles in the forearm. It controls abduction of the thumb, flexion of hand at wrist, flexion of digital phalanx of the fingers, is the sensory nerve for the first three fingers, etc. Because of this major role of the median nerve, it is also called the eye of the hand. If the median nerve is damaged, the ability to abduct and oppose the thumb may be lost due to paralysis of the thenar muscles. Various other symptoms can occur which may be repaired through surgery and tendon transfers. Tendon transfers have been very successful in restoring motor function and improving functional outcomes in patients with median nerve palsy.
Femoral nerve dysfunction, also known as femoral neuropathy, is a rare type of peripheral nervous system disorder that arises from damage to nerves, specifically the femoral nerve. Given the location of the femoral nerve, indications of dysfunction are centered around the lack of mobility and sensation in lower parts of the legs. The causes of such neuropathy can stem from both direct and indirect injuries, pressures and diseases. Physical examinations are usually first carried out, depending on the high severity of the injury. In the cases of patients with hemorrhage, imaging techniques are used before any physical examination. Another diagnostic method, electrodiagnostic studies, are recognized as the gold standard that is used to confirm the injury of the femoral nerve. After diagnosis, different treatment methods are provided to the patients depending upon their symptoms in order to effectively target the underlying causes. Currently, femoral neuropathy is highly underdiagnosed and its precedent medical history is not well documented worldwide.
Deep gluteal syndrome describes the non-discogenic extrapelvic entrapment of the sciatic nerve in the deep gluteal space. In simpler terms this is sciatica due to nerve irritation in the buttocks rather than the spine or pelvis. It is an extension of non-discogenic sciatic nerve entrapment beyond the traditional model of piriformis syndrome. Where sciatic nerve irritation in the buttocks was once thought of as only piriformis muscle, it is now recognized that there are many other causes. Symptoms are pain or dysthesias in the buttocks, hip, and posterior thigh with or without radiating leg pain. Patients often report pain when sitting. The two most common causes are piriformis syndrome and fibrovascular bands, but many other causes exist. Diagnosis is usually done through physical examination, magnetic resonance imaging, magnetic resonance neurography, and diagnostic nerve blocks. Surgical treatment is an endoscopic sciatic nerve decompression where tissue around the sciatic nerve is removed to relieve pressure.