Hypertension is a condition characterized by an elevated blood pressure in which the long term consequences include cardiovascular disease, kidney disease, adrenal gland tumors, vision impairment, memory loss, metabolic syndrome, stroke and dementia. [1] It affects nearly 1 in 2 Americans and remains as a contributing cause of death in the United States. [2] There are many genetic and environmental factors involved with the development of hypertension including genetics, diet, and stress.
Contents
- Hypertension
- Primary and secondary hypertension
- Salt-sensitive hypertension
- Pathophysiology
- Endothelial dysfunction
- Arterial stiffness
- Blood–brain barrier dysfunction
- Inflammation
- Cerebral artery structure and function
- Encephalopathies
- Hypertension and stroke
- Hypertension and vascular dementia
- Hypertension and Alzheimer's disease
- Current treatments
- Lifestyle modifications
- Pharmacological intervention
- References

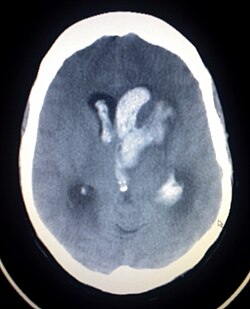
The brain is one of the major organs affected by hypertension and recent findings have linked hypertension to various forms of cognitive decline. Not only does hypertension affect the cellular structure and molecular composition of blood vessels (arteries, veins, capillaries), it also affects their ability to regulate vital functions that are essential for healthy brain function such as oxygen and glucose delivery, cerebral environment control via the blood-brain barrier, and trafficking of immune cells and metabolic by-products. [3] These hypertension-induced effects eventually lead to white matter lesions, which is the pathological basis for hypertension-induced cognitive impairment. [4] A National Institute on Aging (NIA) study that measured cognition twenty years after measuring blood pressure showed that there was a 9% increase in risk for cognitive decline for every 10mmHg increase in systolic blood pressure. [5] Additionally, the Atherosclerosis Risk in Communities cognitive study shows that those with prehypertension or high blood pressure performed lower on processing speed, short-term memory, and executive function tests. [5] Hypertension is also a prominent risk factor for two major brain diseases: stroke and dementia, and accounts for approximately 50% of deaths caused by stroke or heart disease according to the World Health Organization (WHO).