Related Research Articles

The renin–angiotensin system (RAS), or renin–angiotensin–aldosterone system (RAAS), is a hormone system that regulates blood pressure, fluid and electrolyte balance, and systemic vascular resistance.
Diuresis is increased urination (polyuria) or, in the related word senses more often intended, the physiological process that produces such an increase or the administration of medications to encourage that process. It involves extra urine production in the kidneys as part of the body's homeostatic maintenance of fluid balance.
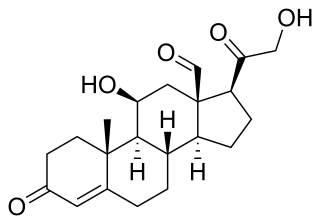
Aldosterone is the main mineralocorticoid steroid hormone produced by the zona glomerulosa of the adrenal cortex in the adrenal gland. It is essential for sodium conservation in the kidney, salivary glands, sweat glands, and colon. It plays a central role in the homeostatic regulation of blood pressure, plasma sodium (Na+), and potassium (K+) levels. It does so primarily by acting on the mineralocorticoid receptors in the distal tubules and collecting ducts of the nephron. It influences the reabsorption of sodium and excretion of potassium (from and into the tubular fluids, respectively) of the kidney, thereby indirectly influencing water retention or loss, blood pressure, and blood volume. When dysregulated, aldosterone is pathogenic and contributes to the development and progression of cardiovascular and kidney disease. Aldosterone has exactly the opposite function of the atrial natriuretic hormone secreted by the heart.

Atrial natriuretic peptide (ANP) or atrial natriuretic factor (ANF) is a natriuretic peptide hormone secreted from the cardiac atria that in humans is encoded by the NPPA gene. Natriuretic peptides are a family of hormone/paracrine factors that are structurally related. The main function of ANP is causing a reduction in expanded extracellular fluid (ECF) volume by increasing renal sodium excretion. ANP is synthesized and secreted by cardiac muscle cells in the walls of the atria in the heart. These cells contain volume receptors which respond to increased stretching of the atrial wall due to increased atrial blood volume.
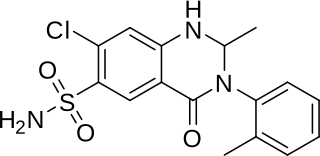
Hydrochlorothiazide is a diuretic medication often used to treat high blood pressure and swelling due to fluid build up. Other uses include treating diabetes insipidus and renal tubular acidosis and to decrease the risk of kidney stones in those with a high calcium level in the urine. Hydrochlorothiazide is less effective than chlortalidone for prevention of heart attack or stroke. Hydrochlorothiazide is taken by mouth and may be combined with other blood pressure medications as a single pill to increase effectiveness.

Diastole is the relaxed phase of the cardiac cycle when the chambers of the heart are re-filling with blood. The contrasting phase is systole when the heart chambers are contracting. Atrial diastole is the relaxing of the atria, and ventricular diastole the relaxing of the ventricles.

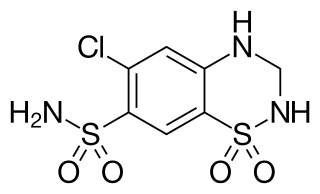
Chlortalidone, also known as chlorthalidone, is a thiazide-like diuretic drug used to treat high blood pressure, swelling including that due to heart failure, liver failure, and nephrotic syndrome, diabetes insipidus, and renal tubular acidosis. Because chlortalidone is reliably effective in most patients with high blood pressure, it is considered a preferred initial treatment. It is also used to prevent calcium-based kidney stones. It is taken by mouth. Effects generally begin within three hours and last for up to three days. Chlortalidone is more effective than hydrochlorothiazide for prevention of heart attack or stroke.

Thiazide refers to both a class of sulfur-containing organic molecules and a class of diuretics based on the chemical structure of benzothiadiazine. The thiazide drug class was discovered and developed at Merck and Co. in the 1950s. The first approved drug of this class, chlorothiazide, was marketed under the trade name Diuril beginning in 1958. In most countries, thiazides are the least expensive antihypertensive drugs available.

Hepatorenal syndrome is a life-threatening medical condition that consists of rapid deterioration in kidney function in individuals with cirrhosis or fulminant liver failure. HRS is usually fatal unless a liver transplant is performed, although various treatments, such as dialysis, can prevent advancement of the condition.

Hydralazine, sold under the brand name Apresoline among others, is a medication used to treat high blood pressure and heart failure. This includes high blood pressure in pregnancy and very high blood pressure resulting in symptoms. It has been found to be particularly useful in heart failure, together with isosorbide dinitrate, for treatment of people of African descent. It is given by mouth or by injection into a vein. Effects usually begin around 15 minutes and last up to six hours.

Metabolic alkalosis is a metabolic condition in which the pH of tissue is elevated beyond the normal range (7.35–7.45). This is the result of decreased hydrogen ion concentration, leading to increased bicarbonate, or alternatively a direct result of increased bicarbonate concentrations. The condition typically cannot last long if the kidneys are functioning properly.
Nephrogenic diabetes insipidus, also known as renal diabetes insipidus, is a form of diabetes insipidus primarily due to pathology of the kidney. This is in contrast to central or neurogenic diabetes insipidus, which is caused by insufficient levels of antidiuretic hormone. Nephrogenic diabetes insipidus is caused by an improper response of the kidney to antidiuretic hormone, leading to a decrease in the ability of the kidney to concentrate the urine by removing free water.
Metolazone is a thiazide-like diuretic marketed under the brand names Zytanix, Metoz, Zaroxolyn, and Mykrox. It is primarily used to treat congestive heart failure and high blood pressure. Metolazone indirectly decreases the amount of water reabsorbed into the bloodstream by the kidney, so that blood volume decreases and urine volume increases. This lowers blood pressure and prevents excess fluid accumulation in heart failure. Metolazone is sometimes used together with loop diuretics such as furosemide or bumetanide, but these highly effective combinations can lead to dehydration and electrolyte abnormalities.

Liddle's syndrome, also called Liddle syndrome, is a genetic disorder inherited in an autosomal dominant manner that is characterized by early, and frequently severe, high blood pressure associated with low plasma renin activity, metabolic alkalosis, low blood potassium, and normal to low levels of aldosterone. Liddle syndrome involves abnormal kidney function, with excess reabsorption of sodium and loss of potassium from the renal tubule, and is treated with a combination of low sodium diet and potassium-sparing diuretics. It is extremely rare, with fewer than 30 pedigrees or isolated cases having been reported worldwide as of 2008.
Pseudohyperaldosteronism is a medical condition which mimics the effects of elevated aldosterone (hyperaldosteronism) by presenting with high blood pressure (hypertension), low blood potassium levels (hypokalemia), metabolic alkalosis, and low levels of plasma renin activity (PRA). However, unlike hyperaldosteronism, this conditions exhibits low or normal levels of aldosterone in the blood. Causes include genetic disorders, acquired conditions, metabolic disorders, and dietary imbalances including excessive consumption of licorice. Confirmatory diagnosis depends on the specific root cause and may involve blood tests, urine tests, or genetic testing; however, all forms of this condition exhibit abnormally low concentrations of both plasma renin activity (PRA) and plasma aldosterone concentration (PAC) which differentiates this group of conditions from other forms of secondary hypertension. Treatment is tailored to the specific cause and focuses on symptom control, blood pressure management, and avoidance of triggers.

Urodilatin (URO) is a hormone that causes natriuresis by increasing renal blood flow. It is secreted in response to increased mean arterial pressure and increased blood volume from the cells of the distal tubule and collecting duct. It is important in oliguric patients as it lowers serum creatinine and increases urine output.
Adolfo José de Bold was an Argentinian-Canadian cardiovascular researcher, best known for his discovery of atrial natriuretic peptide (ANP), a polypeptide hormone secreted by heart muscle cells. The hormone plays a role in regulating blood pressure, blood volume, and cardiovascular growth, and its discovery proved the endocrine function of the heart.
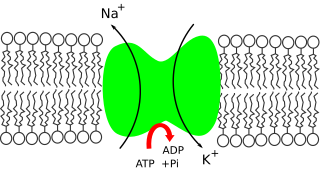
Sodium ions (Na+) are necessary in small amounts for some types of plants, but sodium as a nutrient is more generally needed in larger amounts by animals, due to their use of it for generation of nerve impulses and for maintenance of electrolyte balance and fluid balance. In animals, sodium ions are necessary for the aforementioned functions and for heart activity and certain metabolic functions. The health effects of salt reflect what happens when the body has too much or too little sodium. Characteristic concentrations of sodium in model organisms are: 10mM in E. coli, 30mM in budding yeast, 10mM in mammalian cell and 100mM in blood plasma.

A diuretic is any substance that promotes diuresis, the increased production of urine. This includes forced diuresis. A diuretic tablet is sometimes colloquially called a water tablet. There are several categories of diuretics. All diuretics increase the excretion of water from the body, through the kidneys. There exist several classes of diuretic, and each works in a distinct way. Alternatively, an antidiuretic, such as vasopressin, is an agent or drug which reduces the excretion of water in urine.

Brain natriuretic peptide 32 (BNP), also known as B-type natriuretic peptide, is a hormone secreted by cardiomyocytes in the heart ventricles in response to stretching caused by increased ventricular blood volume. Along with NT-proBNP, BNP is one of two natriuretic peptides.
References
- ↑ "Natriuresis". Merriam-Webster. Retrieved 23 December 2013.
- ↑ Boron, Walter F. and Boulpaep, Emile L. "Medical Physiology". Saunders, 2012, p.1108.
- ↑ Levin ER, Gardner DG, Samson WK (July 1998). "Natriuretic peptides". The New England Journal of Medicine . 339 (5): 321–8. doi:10.1056/NEJM199807303390507. PMID 9682046.
- Further reading
- Granger, JP; Alexander, BT; Llinas, M (2002). "Mechanisms of pressure natriuresis". Current Hypertension Reports. 4 (2): 152–9. doi:10.1007/s11906-002-0040-3. PMID 11884271. S2CID 46323264.
- Hall, J. E.; Mizelle, H. L.; Hildebrandt, D. A.; Brands, M. W. (1990). "Abnormal pressure natriuresis. A cause or a consequence of hypertension?". Hypertension. 15 (6_Pt_1): 547–59. doi: 10.1161/01.HYP.15.6.547 . PMID 1971810.