An arterial blood gas (ABG) test, or arterial blood gas analysis (ABGA) measures the amounts of arterial gases, such as oxygen and carbon dioxide. An ABG test requires that a small volume of blood be drawn from the radial artery with a syringe and a thin needle, but sometimes the femoral artery in the groin or another site is used. The blood can also be drawn from an arterial catheter.
Acidosis is a process causing increased acidity in the blood and other body tissues. If not further qualified, it usually refers to acidity of the blood plasma.
Alkalosis is the result of a process reducing hydrogen ion concentration of arterial blood plasma (alkalemia). In contrast to acidemia, alkalemia occurs when the serum pH is higher than normal. Alkalosis is usually divided into the categories of respiratory alkalosis and metabolic alkalosis or a combined respiratory/metabolic alkalosis.

Metabolic acidosis is a serious electrolyte disorder characterized by an imbalance in the body's acid-base balance. Metabolic acidosis has three main root causes: increased acid production, loss of bicarbonate, and a reduced ability of the kidneys to excrete excess acids. Metabolic acidosis can lead to acidemia, which is defined as arterial blood pH that is lower than 7.35. Acidemia and acidosis are not mutually exclusive – pH and hydrogen ion concentrations also depend on the coexistence of other acid-base disorders; therefore, pH levels in people with metabolic acidosis can range from low to high.

Respiratory acidosis is a state in which decreased ventilation (hypoventilation) increases the concentration of carbon dioxide in the blood and decreases the blood's pH.

Respiratory alkalosis is a medical condition in which increased respiration elevates the blood pH beyond the normal range (7.35–7.45) with a concurrent reduction in arterial levels of carbon dioxide. This condition is one of the four primary disturbance of acid–base homeostasis.
The anion gap is a value calculated from the results of multiple individual medical lab tests. It may be reported with the results of an electrolyte panel, which is often performed as part of a comprehensive metabolic panel.

Metabolic alkalosis is a metabolic condition in which the pH of tissue is elevated beyond the normal range (7.35–7.45). This is the result of decreased hydrogen ion concentration, leading to increased bicarbonate, or alternatively a direct result of increased bicarbonate concentrations. The condition typically cannot last long if the kidneys are functioning properly.
Hyperchloremic acidosis is a form of metabolic acidosis associated with a normal anion gap, a decrease in plasma bicarbonate concentration, and an increase in plasma chloride concentration. Although plasma anion gap is normal, this condition is often associated with an increased urine anion gap, due to the kidney's inability to secrete ammonia.
In renal physiology, net acid excretion (NAE) is the net amount of acid excreted in the urine per unit time. Its value depends on urine flow rate, urine acid concentration, and the concentration of bicarbonate in the urine. NAE is commonly expressed in units of milliliters per minute (ml/min) and is given by the following equation:
Acid–base homeostasis is the homeostatic regulation of the pH of the body's extracellular fluid (ECF). The proper balance between the acids and bases in the ECF is crucial for the normal physiology of the body—and for cellular metabolism. The pH of the intracellular fluid and the extracellular fluid need to be maintained at a constant level.
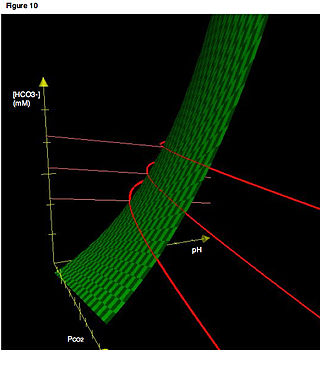
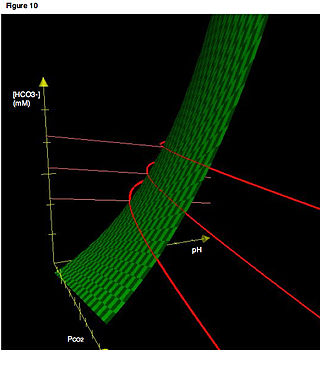
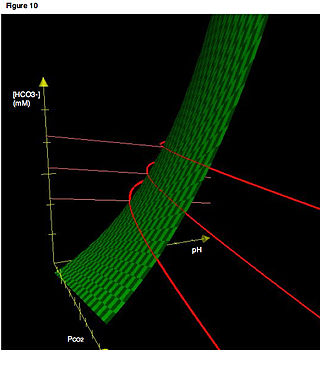
In acid base physiology, the Davenport diagram is a graphical tool, developed by Horace W. Davenport, that allows a clinician or investigator to describe blood bicarbonate concentrations and blood pH following a respiratory and/or metabolic acid-base disturbance. The diagram depicts a three-dimensional surface describing all possible states of chemical equilibria between gaseous carbon dioxide, aqueous bicarbonate and aqueous protons at the physiologically complex interface of the alveoli of the lungs and the alveolar capillaries. Although the surface represented in the diagram is experimentally determined, the Davenport diagram is rarely used in the clinical setting, but allows the investigator to envision the effects of physiological changes on blood acid-base chemistry. For clinical use there are two recent innovations: an Acid-Base Diagram which provides Text Descriptions for the abnormalities and a High Altitude Version that provides text descriptions appropriate for the altitude.
Contraction alkalosis refers to the increase in blood pH that occurs as a result of fluid losses. The change in pH is especially pronounced with acidic fluid losses caused by problems like vomiting.
Renal compensation is a mechanism by which the kidneys can regulate the plasma pH. It is slower than respiratory compensation, but has a greater ability to restore normal values.
Respiratory compensation is the modulation by the brainstem respiratory centers, which involves altering alveolar ventilation to try and bring the plasma pH back to its normal value (7.4) in order to keep the acid-base balance in the body. It usually occurs within minutes to hours and is much faster than renal compensation, but has less ability to restore normal values.
Normal anion gap acidosis is an acidosis that is not accompanied by an abnormally increased anion gap.
Acid–base imbalance is an abnormality of the human body's normal balance of acids and bases that causes the plasma pH to deviate out of the normal range. In the fetus, the normal range differs based on which umbilical vessel is sampled. It can exist in varying levels of severity, some life-threatening.

High anion gap metabolic acidosis is a form of metabolic acidosis characterized by a high anion gap. Metabolic acidosis occurs when the body produces too much acid, or when the kidneys are not removing enough acid from the body. Several types of metabolic acidosis occur, grouped by their influence on the anion gap.
Winter's formula, named after Dr. R.W. Winters, is a formula used to evaluate respiratory compensation when analyzing acid-base disorders and a metabolic acidosis is present. It can be given as
Delta ratio, or "delta-delta", is a formula that can be used to assess elevated anion gap metabolic acidosis and to evaluate whether a mixed acid–base disorder is present. The anion gap (AG) without potassium is calculated first and if a metabolic acidosis is present, results in either a high anion gap metabolic acidosis (HAGMA) or a normal anion gap acidosis (NAGMA). A low anion gap is usually an oddity of measurement, rather than a clinical concern.