Diabetes insipidus (DI) is a condition characterized by large amounts of dilute urine and increased thirst. The amount of urine produced can be nearly 20 liters per day. Reduction of fluid has little effect on the concentration of the urine. Complications may include dehydration or seizures.

Clinical chemistry is a division in medical laboratory sciences focusing on qualitative tests of important compounds, referred to as analytes or markers, in bodily fluids and tissues using analytical techniques and specialized instruments. This interdisciplinary field includes knowledge from medicine, biology, chemistry, biomedical engineering, informatics, and an applied form of biochemistry.
Liver function tests, also referred to as a hepatic panel, are groups of blood tests that provide information about the state of a patient's liver. These tests include prothrombin time (PT/INR), activated partial thromboplastin time (aPTT), albumin, bilirubin, and others. The liver transaminases aspartate transaminase and alanine transaminase are useful biomarkers of liver injury in a patient with some degree of intact liver function.

Nephrotic syndrome is a collection of symptoms due to kidney damage. This includes protein in the urine, low blood albumin levels, high blood lipids, and significant swelling. Other symptoms may include weight gain, feeling tired, and foamy urine. Complications may include blood clots, infections, and high blood pressure.

The blood sugar level, blood sugar concentration, blood glucose level, or glycemia is the measure of glucose concentrated in the blood. The body tightly regulates blood glucose levels as a part of metabolic homeostasis.

Hyperparathyroidism is an increase in parathyroid hormone (PTH) levels in the blood. This occurs from a disorder either within the parathyroid glands or as response to external stimuli. Symptoms of hyperparathyroidism are caused by inappropriately normal or elevated blood calcium excreted from the bones and flowing into the blood stream in response to increased production of parathyroid hormone. In healthy people, when blood calcium levels are high, parathyroid hormone levels should be low. With long-standing hyperparathyroidism, the most common symptom is kidney stones. Other symptoms may include bone pain, weakness, depression, confusion, and increased urination. Both primary and secondary may result in osteoporosis.

The endocrine system is a network of glands and organs located throughout the body. It is similar to the nervous system in that it plays a vital role in controlling and regulating many of the body's functions. Endocrine glands are ductless glands of the endocrine system that secrete their products, hormones, directly into the blood. The major glands of the endocrine system include the pineal gland, pituitary gland, pancreas, ovaries, testicles, thyroid gland, parathyroid gland, hypothalamus and adrenal glands. The hypothalamus and pituitary glands are neuroendocrine organs.

Diabetic nephropathy, also known as diabetic kidney disease, is the chronic loss of kidney function occurring in those with diabetes mellitus. Diabetic nephropathy is the leading causes of chronic kidney disease (CKD) and end-stage renal disease (ESRD) globally. The triad of protein leaking into the urine, rising blood pressure with hypertension and then falling renal function is common to many forms of CKD. Protein loss in the urine due to damage of the glomeruli may become massive, and cause a low serum albumin with resulting generalized body swelling (edema) so called nephrotic syndrome. Likewise, the estimated glomerular filtration rate (eGFR) may progressively fall from a normal of over 90 ml/min/1.73m2 to less than 15, at which point the patient is said to have end-stage renal disease. It usually is slowly progressive over years.
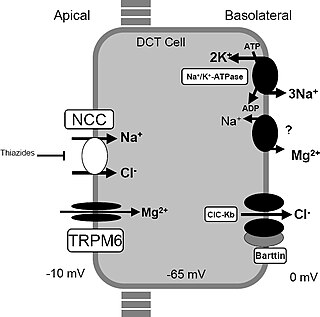
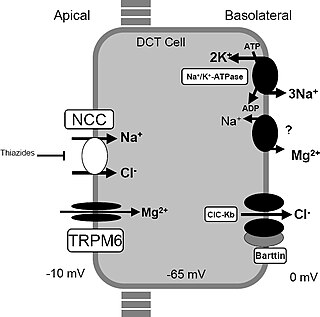
Gitelman syndrome (GS) is an autosomal recessive kidney tubule disorder characterized by low blood levels of potassium and magnesium, decreased excretion of calcium in the urine, and elevated blood pH. It is the most frequent hereditary salt-losing tubulopathy. Gitelman syndrome is caused by disease-causing variants on both alleles of the SLC12A3 gene. The SLC12A3 gene encodes the thiazide-sensitive sodium-chloride cotransporter, which can be found in the distal convoluted tubule of the kidney.

Respiratory alkalosis is a medical condition in which increased respiration elevates the blood pH beyond the normal range (7.35–7.45) with a concurrent reduction in arterial levels of carbon dioxide. This condition is one of the four primary disturbances of acid–base homeostasis.

Nephritic syndrome is a syndrome comprising signs of nephritis, which is kidney disease involving inflammation. It often occurs in the glomerulus, where it is called glomerulonephritis. Glomerulonephritis is characterized by inflammation and thinning of the glomerular basement membrane and the occurrence of small pores in the podocytes of the glomerulus. These pores become large enough to permit both proteins and red blood cells to pass into the urine. By contrast, nephrotic syndrome is characterized by proteinuria and a constellation of other symptoms that specifically do not include hematuria. Nephritic syndrome, like nephrotic syndrome, may involve low level of albumin in the blood due to the protein albumin moving from the blood to the urine.
A metabolic disorder is a disorder that negatively alters the body's processing and distribution of macronutrients, such as proteins, fats, and carbohydrates. Metabolic disorders can happen when abnormal chemical reactions in the body alter the normal metabolic process. It can also be defined as inherited single gene anomaly, most of which are autosomal recessive.
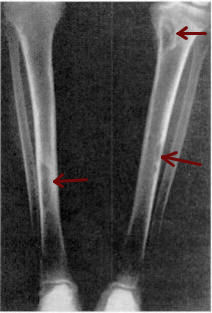
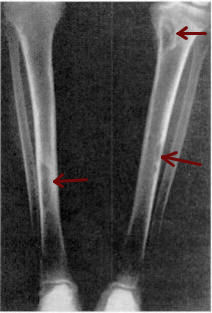
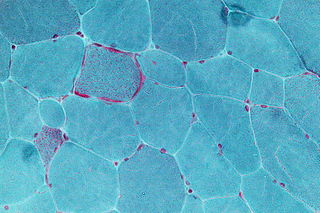
Osteitis fibrosa cystica is a skeletal disorder resulting in a loss of bone mass, a weakening of the bones as their calcified supporting structures are replaced with fibrous tissue, and the formation of cyst-like brown tumors in and around the bone. Osteitis fibrosis cystica (OFC), also known as osteitis fibrosa, osteodystrophia fibrosa, and von Recklinghausen's disease of bone, is caused by hyperparathyroidism, which is a surplus of parathyroid hormone from over-active parathyroid glands. This surplus stimulates the activity of osteoclasts, cells that break down bone, in a process known as osteoclastic bone resorption. The hyperparathyroidism can be triggered by a parathyroid adenoma, hereditary factors, parathyroid carcinoma, or renal osteodystrophy. Osteoclastic bone resorption releases minerals, including calcium, from the bone into the bloodstream, causing both elevated blood calcium levels, and the structural changes which weaken the bone. The symptoms of the disease are the consequences of both the general softening of the bones and the excess calcium in the blood, and include bone fractures, kidney stones, nausea, moth-eaten appearance in the bones, appetite loss, and weight loss.

Hypoalbuminemia is a medical sign in which the level of albumin in the blood is low. This can be due to decreased production in the liver, increased loss in the gastrointestinal tract or kidneys, increased use in the body, or abnormal distribution between body compartments. Patients often present with hypoalbuminemia as a result of another disease process such as malnutrition as a result of severe anorexia nervosa, sepsis, cirrhosis in the liver, nephrotic syndrome in the kidneys, or protein-losing enteropathy in the gastrointestinal tract. One of the roles of albumin is being the major driver of oncotic pressure in the bloodstream and the body. Thus, hypoalbuminemia leads to abnormal distributions of fluids within the body and its compartments. As a result, associated symptoms include edema in the lower legs, ascites in the abdomen, and effusions around internal organs. Laboratory tests aimed at assessing liver function diagnose hypoalbuminemia. Once identified, it is a poor prognostic indicator for patients with a variety of different diseases. Yet, it is only treated in very specific indications in patients with cirrhosis and nephrotic syndrome. Treatment instead focuses on the underlying cause of the hypoalbuminemia. Albumin is an acute negative phase respondent and not a reliable indicator of nutrition status.
Nephrogenic diabetes insipidus, recently renamed arginine vasopressin resistance (AVP-R) and previously known as renal diabetes insipidus, is a form of diabetes insipidus primarily due to pathology of the kidney. This is in contrast to central or neurogenic diabetes insipidus, which is caused by insufficient levels of vasopressin. Nephrogenic diabetes insipidus is caused by an improper response of the kidney to vasopressin, leading to a decrease in the ability of the kidney to concentrate the urine by removing free water.
Phosphate nephropathy or nephrocalcinosis is an adverse renal condition that arises with a formation of phosphate crystals within the kidney's tubules. This renal insufficiency is associated with the use of oral sodium phosphate (OSP) such as C.B. Fleet's Phospho soda and Salix's Visocol, for bowel cleansing prior to a colonoscopy.

Milk-alkali syndrome (MAS), also referred to as calcium-alkali syndrome, is the third most common cause of elevated blood calcium levels (hypercalcemia). Milk-alkali syndrome is characterized by hypercalcemia, metabolic alkalosis, and acute kidney injury.
A basic metabolic panel (BMP) is a blood test consisting of a set of seven or eight biochemical tests and is one of the most common lab tests ordered by health care providers. Outside the United States, blood tests made up of the majority of the same biochemical tests are called urea and electrolytes, or urea, electrolytes, creatinine, and are often referred to as 'kidney function tests' as they also include a calculated estimated glomerular filtration rate. The BMP provides key information regarding fluid and electrolyte status, kidney function, blood sugar levels, and response to various medications and other medical therapies. It is frequently employed as a screening tool during a physical exam.
Recombinant human parathyroid hormone, sold under the brand name Preotact among others, is an artificially manufactured form of the parathyroid hormone used to treat hypoparathyroidism. Recombinant human parathyroid hormone is used in the treatment of osteoporosis in postmenopausal women at high risk of osteoporotic fractures. A significant reduction in the incidence of vertebral fractures has been demonstrated. It is used in combination with calcium and vitamin D supplements.
Post-mortem chemistry, also called necrochemistry or death chemistry, is a subdiscipline of chemistry in which the chemical structures, reactions, processes and parameters of a dead organism is investigated. Post-mortem chemistry plays a significant role in forensic pathology. Biochemical analyses of vitreous humor, cerebrospinal fluid, blood and urine is important in determining the cause of death or in elucidating forensic cases.